TX HHS Form 1031. Case Record Transfer
The TX HHS Form 1031, Case Record Transfer, helps solve the problem of transferring case records between offices or caseworkers.
TX HHS Form 1028. Medically Fragile Group Criteria Certification
The TX HHS Form 1028, Medically Fragile Group Criteria Certification, is a crucial document that helps solve the problem of identifying individuals who require specialized care.
TX HHS Form 1027. Caregiver Status Questionnaire
The TX HHS Form 1027, Caregiver Status Questionnaire, is a valuable tool for understanding the needs and circumstances of caregivers providing unpaid care to individuals in need.
TX HHS Form 1026-TSI. Verification of Railroad Retirement Benefits - TSI
The TX HHS Form 1026-TSI, Verification of Railroad Retirement Benefits - TSI, is a crucial document that helps individuals verify their railroad retirement benefits.
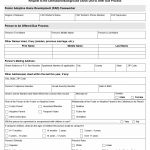
TX HHS Form 2919. Request for a Registration Permit
The TX HHS Form 2919, Request for a Registration Permit, is a crucial document that helps solve the problem of obtaining a registration permit for child care services. This form is typically used by individuals or organizations seeking to operate a child care facility in Texas.
TX HHS Form 2910. CCR Application for a License or Certification to Operate a Child Day Care Facility
The TX HHS Form 2910, CCR Application for a License or Certification to Operate a Child Day Care Facility, is a crucial document that helps solve the problem of obtaining a license or certification to operate a child care center, school-age program, before- or after-school program, or child care
TX HHS Form 2907. CCR Statement of Foster Parent and Child-Placing Agency Rights and Responsibilities
The TX HHS Form 2907, CCR Statement of Foster Parent and Child-Placing Agency Rights and Responsibilities, is a crucial document that helps foster parents and child-placing agencies clarify their roles and responsibilities in the foster care process.
TX HHS Form 2906. Child Placing Agency Internal Investigation Report
The TX HHS Form 2906, Child Placing Agency Internal Investigation Report, is a valuable tool for resolving allegations or incidents within child placing agencies.
TX HHS Form 2900. Request to the Centralized Background Check Unit to Offer Due Process
The TX HHS Form 2900, "Request to the Centralized Background Check Unit to Offer Due Process," is a crucial document for foster care and adoption agencies.
TX HHS Form 2885. Childrens Products Certification
The TX HHS Form 2885, Children's Products Certification, is a crucial document for child care centers and homes to ensure the safety of children.