TX HHS Form H2067-MC. Managed Care Programs Communication
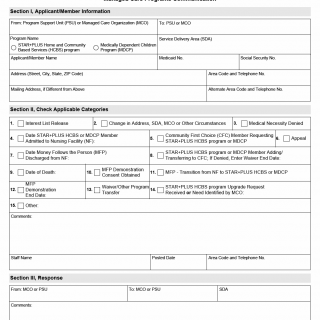
Form H2067-MC, titled “Managed Care Programs Communication,” is an official Texas Health and Human Services (HHS) document used to exchange critical information between a Managed Care Organization (MCO) and the Program Support Unit (PSU). The form plays a coordinating role in managed care programs such as STAR+PLUS Home and Community Based Services (HCBS) and the Medically Dependent Children Program (MDCP).
Its main purpose is to formally notify involved parties about changes, decisions, requests, and significant events affecting an applicant or enrolled member. Without this form, many program actions cannot be properly tracked or processed.
Purpose and When This Form Is Used
Form H2067-MC is used whenever structured communication is required between an MCO and PSU regarding a member’s status or program-related event. It is not a general application form, but rather an operational communication tool.
This form is required in situations such as changes in address or managed care organization, program eligibility decisions, appeals, nursing facility admissions or discharges, and transitions between waiver programs.
Who Can Complete and Submit This Form
This form is completed by authorized staff members of:
- Managed Care Organizations (MCOs)
- Program Support Units (PSUs)
Applicants or members themselves do not usually fill out this form directly. It is prepared and submitted by program staff acting on their behalf.
Explanation of Key Sections
Section I – Applicant/Member Information
This section identifies the individual affected by the communication. It includes the program name (STAR+PLUS HCBS or MDCP), service delivery area (SDA), and personal identifiers such as Medicaid number, Social Security number, and contact details.
Accurate identification is essential, as errors here can result in delays or misapplied actions.
Section II – Applicable Categories
This section defines the reason for the communication. Staff must check one or more categories that describe the situation, such as:
- Interest list release
- Change in address, SDA, or MCO
- Medical necessity denial
- Nursing facility admission or discharge dates
- Community First Choice (CFC) requests or transfers
- Appeals
- Money Follows the Person (MFP) transitions
- Waiver program transfers or upgrades
- Date of death
A comments field allows staff to clarify details that do not fit neatly into a single category.
Section III – Response
This section is used by the receiving party to document their response. It confirms receipt, provides additional comments, and records follow-up actions. Staff contact details and posting dates help maintain accountability.
Legislative and Program Context
Form H2067-MC is required under Texas Medicaid managed care administrative procedures. Programs such as STAR+PLUS HCBS, MDCP, Community First Choice, and Money Follows the Person rely on documented inter-agency communication to meet state and federal oversight requirements.
Using this form ensures compliance with Medicaid waiver rules, program integrity standards, and continuity-of-care obligations.
Practical Tips for Completing the Form
- Verify Medicaid and Social Security numbers before submission.
- Select all applicable categories in Section II to avoid incomplete processing.
- Use the comments field to explain complex situations or timelines.
- Always include staff contact information in case clarification is needed.
- Ensure dates are consistent across related program records.
Common Mistakes to Avoid
- Leaving the applicable category section incomplete.
- Using outdated contact or address information.
- Failing to document nursing facility admission or discharge dates.
- Submitting the form without clear comments for non-standard cases.
Real-Life Use Examples
- An MCO notifies the PSU that a STAR+PLUS HCBS member has been admitted to a nursing facility.
- A PSU informs an MCO of an approved appeal affecting MDCP services.
- An MCO documents a member’s transition from a nursing facility back to community-based care under the MFP program.
Documents Commonly Referenced with This Form
- Eligibility determinations
- Medical necessity decisions
- Appeal documentation
- Nursing facility admission or discharge records
- Waiver transfer approvals
Frequently Asked Questions
Is Form H2067-MC required for every program change?
It is required whenever formal communication between an MCO and PSU is needed to document a change or decision.
Can members submit this form themselves?
No. The form is completed by authorized program staff.
What programs use this form?
It is primarily used for STAR+PLUS HCBS, MDCP, Community First Choice, and related Medicaid waiver programs.
What happens if the form is not submitted?
Program actions may be delayed, denied, or incorrectly recorded.
Can multiple categories be selected?
Yes. All applicable categories should be checked.
Micro-FAQ
- Purpose: Official communication between MCOs and PSUs.
- Who files: Authorized MCO or PSU staff.
- Deadline: As soon as the event or change occurs.
- Attachments: Supporting program or eligibility records.
- Submitted to: Program Support Unit or Managed Care Organization.
Related Forms and Programs
- STAR+PLUS HCBS enrollment and change forms
- MDCP eligibility and appeal forms
- Community First Choice documentation
- Money Follows the Person transition forms
Form Details
- Form Name: Managed Care Programs Communication
- Form Number: H2067-MC
- Program: STAR+PLUS HCBS, MDCP
- State: Texas
- Revision Date: September 2017