TX HHS Form 6109. Special Care Facility Incident Report
Form 6109, officially titled Special Care Facility Incident Report, is a mandatory document used by special care facilities to report serious events such as abuse, neglect, fires, injuries, medical emergencies, and other incidents affecting patients or staff. The form is designed to help regulatory authorities track safety issues, ensure timely intervention, and prevent future harm. Although the form looks straightforward, completing it accurately requires attention to detail and an understanding of reporting requirements.
Purpose of Form 6109
The form serves as the primary reporting mechanism for incidents that jeopardize patient safety or indicate possible violations of care standards. State regulations require prompt reporting to ensure that vulnerable individuals—children, elderly adults, and people with disabilities—receive protection from harm. The form also acts as an internal record that facilities can use to analyze risks, implement corrective actions, and demonstrate compliance.
When Filing Is Mandatory
- Immediately (as soon as possible): Any suspected or confirmed abuse, neglect, or exploitation involving a child, elderly person, or disabled individual.
- Within 24 hours: Any fire that caused injury or death.
- Within 10 calendar days: Any fire event, even if no injuries occurred.
Failure to file on time can lead to regulatory penalties, heightened scrutiny, and potential legal liability for the facility.
Explanation of Key Sections
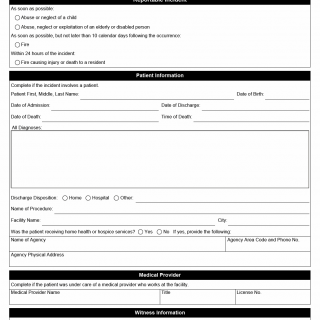
1. Patient Information
This section documents the patient affected by the incident. It includes identifying information, admission and discharge dates, diagnoses, procedures, and whether the patient was receiving home health or hospice services.
- What this section establishes: The patient’s medical status before and after the incident, which helps evaluate the severity and impact.
- Frequent mistakes: Leaving diagnosis fields blank, incorrect discharge dispositions, missing middle names leading to identification issues.
2. Medical Provider
Used when the patient was under the care of an on-site licensed provider. This ensures regulatory bodies know which professional supervised treatment and whether provider negligence is a factor.
3. Witness Information
Completed only when staff members witnessed the incident. Witness accounts often become critical in investigations, especially for abuse or neglect cases.
4. Alleged Perpetrator Information
This section is necessary when the incident involves potential wrongdoing by a staff member. Detailed identification is essential for law enforcement and licensing agencies.
- Common errors: Missing license numbers, incomplete addresses, providing only a nickname.
5. Summary of the Incident
The heart of the report. Facilities must describe what happened, who was involved, actions taken, and the timeline of discovery. Regulators rely heavily on this narrative to assess the urgency and seriousness of the incident.
6. Diagnostic Tests & Treatment
If the patient received treatment or diagnostic imaging, report all procedures and test results. This helps demonstrate whether appropriate medical intervention was delivered promptly.
7. Investigation Narrative
This narrative outlines the facility’s internal response, including steps taken to prevent recurrence. It is essential for quality assurance reviews and state compliance evaluations.
8. Referrals
Facilities must list all external reports sent to authorities such as the FDA, Police Department, OSHA, Medical Board, Nursing Board, Pharmacy Board, or Adult/Child Protective Services.
9. Actions to Be Taken
This checklist reflects the corrective measures the facility intends to implement. These may include staff training, disciplinary action, policy updates, or quality monitoring.
Practical Recommendations
- Record the incident details immediately while information is fresh.
- Verify all names, dates, and license numbers to avoid investigation delays.
- Attach supplemental narrative sheets when the incident is complex.
- For abuse allegations, ensure the alleged perpetrator does not interact with the patient during the investigation.
- Document all communication with protective services or law enforcement.
Examples of Real-World Situations
- Example 1: A resident with dementia falls unattended and suffers a fracture—requires immediate reporting and investigation.
- Example 2: A staff member notices unexplained bruising on an elderly patient—suspected abuse triggers immediate mandatory reporting.
- Example 3: A small electrical fire occurs in a storage room—requires filing within 10 days even if no injuries occurred.
- Example 4: A medication misadministration leads to emergency hospitalization—requires treatment documentation and quality review.
Documents Commonly Attached
- Witness statements
- Medical treatment notes
- Diagnostic test results
- Photographs of injuries or damage
- Copies of reports filed with law enforcement or protective services
FAQ
- Who must file Form 6109? Any licensed special care facility handling the incident must file the report.
- What if multiple patients were involved? File a separate form for each affected individual.
- Are verbal reports enough? No, written documentation using Form 6109 is required for compliance.
- What if the incident is still under investigation? File the initial report and later submit supplemental documentation.
- Do minor injuries need reporting? Only injuries requiring treatment or those tied to abuse/neglect allegations.
- Can families request copies? Yes, but the facility must follow privacy and record-release regulations.
Micro-FAQ (Short Answers)
- Purpose? To document critical safety incidents in special care facilities.
- Who files? Facility administrators or designated compliance staff.
- Deadline? Immediately for abuse; 24 hours for fire injuries; 10 days for all fires.
- Attachments? Witness statements, test results, medical notes.
- Submitted to? Appropriate state regulatory agency.
- Includes patient info? Yes, when a patient is involved.
- Includes staff info? Yes, for witnesses or alleged perpetrators.
- Requires narrative? Yes, a detailed account of events and actions.
Related Forms
- Special Care Facility Safety Checklist
- Abuse and Neglect Reporting Form
- Healthcare Provider Incident Statement
- Fire Incident Supplemental Report
Form Details
- Form Name: Special Care Facility Incident Report
- Form Number: 6109
- Edition: October 2024
- Region: United States / State regulatory agencies