TX HHS Form 3608. Individual Plan of Care (IPC) HCS and CFC
Form 3608 is an official planning and authorization document used in Texas Medicaid programs for individuals receiving services through Home and Community-based Services (HCS) and Community First Choice (CFC). The form documents an individual’s approved services, service levels, providers, and funding sources for a specific period of time, ensuring that care is appropriate, necessary, and compliant with state requirements.
This form plays a central role in coordinating services, approving changes, and protecting the health, safety, and rights of the person receiving services.
Purpose of Form 3608
The primary purpose of Form 3608 is to formally establish or update an Individual Plan of Care (IPC). The IPC outlines what services a person will receive, who will provide them, how often they will be delivered, and under which funding source.
The form is required to:
- Authorize Medicaid-funded HCS and CFC services
- Document service levels and approved units
- Support person-directed planning decisions
- Ensure services are medically and functionally necessary
- Maintain compliance with Texas Medicaid rules
When This Form Is Required
Form 3608 must be completed in several specific situations:
- Initial enrollment into HCS or CFC services
- Annual IPC renewal
- Transfer between providers or service delivery options
- Revisions due to changes in the Person-Directed Plan (PDP)
- Emergency revisions meeting state emergency criteria
- Approved increases or decreases in authorized services
The form is not required for informal support changes or services paid entirely by non-Medicaid funding unless they affect the authorized Medicaid services.
Who Is Authorized to Complete and Sign the Form
Form 3608 is completed collaboratively by the service planning team. This typically includes:
- The person receiving services or their Legally Authorized Representative (LAR)
- The HCS or CFC program provider
- The Local Intellectual and Developmental Disability Authority (LIDDA) or Service Coordinator (SC)
Required signatures depend on the type of IPC action being taken. Some revisions allow limited processing without a full IPC meeting, while others require full participation and signatures from all parties.
Explanation of Key Sections
Individual and Program Information
This section identifies the person receiving services, including Medicaid number, dates of coverage, address, age, level of need, county of service, and residential setting. Accuracy here is critical, as errors can delay authorization or payment.
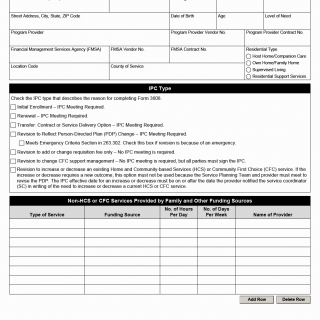
IPC Type
This section explains why the form is being completed, such as initial enrollment, renewal, transfer, or revision. Selecting the correct IPC type determines whether a meeting is required and how the change is processed.
Non-HCS or CFC Services
This area documents services provided by family members or other funding sources. While not Medicaid-funded, these services help demonstrate that Medicaid services are not duplicating other supports.
HCS Services
This section lists all authorized HCS services, including adaptive aids, nursing, therapies, residential supports, respite, and employment services. For revisions, providers must indicate whether services are being increased or decreased.
Consumer Directed Services (CDS)
If the person uses CDS, this section documents self-directed services, authorized units, and approved funding amounts, including Financial Management Services (FMS).
CFC Services
This section covers CFC services such as personal assistance, habilitation, emergency response services, and CFC support management, including whether services are delivered through CDS.
Certifications and Signatures
This section confirms that the person or LAR was informed of rights, complaint processes, and provider choice. Signatures certify that services are necessary, appropriate, cost-effective, and not available through other funding sources.
LIDDA or Service Coordinator Response
For service increases or decreases, the Service Coordinator documents whether an IPC meeting is required and confirms participation or approval timelines.
Practical Tips for Completing Form 3608
- Verify Medicaid numbers, dates, and service codes before submission.
- Select the correct IPC type to avoid unnecessary delays.
- Ensure increases or decreases align with written notification dates.
- Confirm required signatures based on the type of revision.
- Keep copies of all signed forms for records and audits.
Common Mistakes to Avoid
- Using the wrong IPC type for the situation
- Failing to document emergency criteria correctly
- Missing required signatures or dates
- Authorizing services not supported by the PDP
- Incorrect service codes or units
Legal and Regulatory Context
Form 3608 is required under Texas Medicaid program rules governing HCS and CFC services. State regulations require documented service planning to ensure that services protect health and welfare, support community integration, and comply with cost-effectiveness standards. The IPC serves as a legally recognized authorization for Medicaid-funded services.
Real-Life Situations Where This Form Is Used
- An individual enrolls in HCS services for the first time after Medicaid eligibility is approved.
- A provider requests additional nursing hours due to a medical change.
- A person transfers to a new provider and requires a revised IPC.
- CFC support management services are added without changing other services.
Documents Commonly Needed with This Form
- Person-Directed Plan (PDP)
- Service Coordinator notifications
- Emergency justification documentation (if applicable)
- Provider service agreements
- Supporting assessments or evaluations
Frequently Asked Questions
Is Form 3608 required every year?
Yes, an IPC renewal is required annually to continue authorized services.
Can services be increased without an IPC meeting?
Some increases may not require a meeting, depending on state rules and documentation.
Who signs the IPC?
The person or LAR, the provider, and sometimes the Service Coordinator.
What happens if information is incorrect?
Errors can delay authorization or result in denied claims.
Is this form used for non-Medicaid services?
No, it authorizes Medicaid-funded HCS and CFC services.
Related Forms
- Person-Directed Plan (PDP)
- Service Coordinator Notification Forms
- HCS Enrollment Forms
- CFC Support Management Documentation
Form Details
- Form Name: Individual Plan of Care (IPC)
- Form Number: 3608
- Programs: HCS and Community First Choice (CFC)
- State: Texas
- Revision Date: January 2025