TX HHS Form 3599. Habilitation Service Provider Orientation/Supervisory Visits
Texas Form 3599 is an official document used by providers within the Texas Health and Human Services Commission (HHSC) programs, specifically CLASS (Community Living Assistance and Support Services) and CFC (Community First Choice). The form is titled “Habilitation Service Provider Orientation / Supervisory Visits” and serves two major functions: documenting the provider’s initial orientation to the individual’s needs, and recording ongoing supervisory visits to ensure service quality and compliance.
Why This Form Matters (Purpose and Legal Requirement)
Texas regulations require providers to deliver habilitation and PAS/HAB services strictly according to the individual’s approved plan and state program standards. Form 3599 acts as proof that the service provider has received the necessary orientation, understands the individual’s needs, is aware of safety protocols, and is being periodically supervised. Without this form, agencies cannot demonstrate compliance with state documentation requirements for CLASS and CFC programs.
Who Must Use It and When
- Habilitation or PAS/HAB service providers assigned to individuals in CLASS or CFC.
- Before a new provider begins services — orientation must be documented.
- Whenever a provider is reassigned or returns after a long break.
- During each supervisory visit to verify service quality, accuracy of tasks performed, and any changes in the individual’s needs.
What the Form Contains — Section-by-Section Explanation
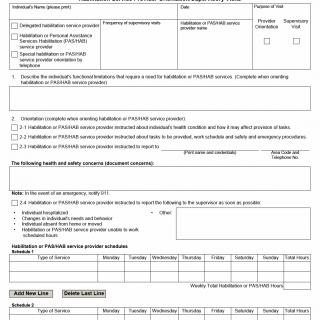
Orientation Section
- Individual’s functional limitations: A narrative description explaining why habilitation or PAS/HAB services are needed — mobility issues, communication difficulties, cognitive limitations, or medical conditions.
- Instruction record: Documentation that the provider was instructed on the individual’s health status, care tasks, schedule, safety procedures, and expectations.
- Safety concerns: Noting any risks or critical information. Providers must be briefed on when emergency services (such as 911) should be contacted.
- Reporting procedures: Clear instructions on whom to notify if the individual is hospitalized, experiences behavior changes, is absent from home, or if the provider cannot work scheduled hours.
Service Schedule
The weekly schedule outlines when and what type of services will be delivered each day. This clarifies responsibilities and ensures alignment with the approved care plan. It also prevents misunderstandings about expected service hours.
Supervisory Visit / Task Performance
- Task checklist: Areas such as hygiene, dressing, meal preparation, feeding, exercise, cleaning, community assistance, mobility, and health-related tasks are evaluated as satisfactory (S) or unsatisfactory (U).
- Competency evaluation: Supervisors assess whether the provider can perform standard and delegated tasks safely and correctly.
- Feedback from the individual or LAR: Used to confirm satisfaction and note any concerns.
- Compliance review: Verification that the provider follows the established schedule.
- Service delivery issues: Any problems, training needs, or corrective actions are documented for transparency and follow-up.
- Continuation of services: Supervisor indicates whether the individual still requires the same level of support.
Common Mistakes & Pitfalls
- Leaving orientation questions blank, especially functional limitations.
- Writing vague descriptions instead of clear, specific information.
- Failing to update the form when an individual’s condition changes.
- Incorrect or incomplete service hours in the weekly schedule.
- Missing signatures from the provider, supervisor, or the individual/LAR.
Practical Advice for Filling Out Form 3599
- Explain limitations and tasks in detail — include what the individual can and cannot do independently.
- Make sure the provider understands safety procedures before services begin.
- Check accuracy of the weekly schedule — mismatched hours often cause service disputes.
- During supervisory visits, evaluate each task based on direct observation or discussion.
- Document all training needs promptly — this protects both the provider and the agency.
- Keep a copy of each completed form for future audits.
Real-Life Scenarios Where Form 3599 Is Used
- Scenario 1: A provider is newly assigned to an adult with mobility limitations. Form 3599 records the orientation, including instructions on safe transfers, meal preparation assistance, and emergency steps.
- Scenario 2: An individual under CLASS receives a new habilitation provider. The form documents health conditions, behavior support instructions, and daily tasks the provider must follow.
- Scenario 3: During a supervisory visit, the supervisor notices that cleaning tasks are not performed adequately. Form 3599 documents this issue along with corrective actions.
- Scenario 4: The individual’s needs change after hospitalization. A new Form 3599 is completed to update tasks, safety requirements, and the provider’s schedule.
Documents Commonly Attached
- Individual Plan of Care (IPC)
- Service Delivery Plan or Task List
- Behavior Support Plan (if applicable)
- Medical summaries or physician orders related to health-related tasks
- Emergency contact sheet
FAQ
- Who fills out Form 3599? The supervisor or service coordinator completes it, with signatures from the provider and the individual or their representative.
- When is orientation required? Before a provider begins delivering habilitation or PAS/HAB services.
- How often are supervisory visits documented? As required by the individual's plan and agency policy—typically every few months or when conditions change.
- Can this form be updated? Yes, any time the individual’s needs, tasks, or provider assignment changes.
- Is Form 3599 required for all CLASS/CFC providers? Yes, it documents mandatory orientation and supervision.
- What happens if the form is incomplete? It may result in compliance issues or delays in service authorization.
- Does the individual need to sign it? Yes, unless they have a legally authorized representative who signs instead.
Micro-FAQ
- Purpose? To document provider orientation and supervisory visits.
- Who completes it? Supervisor or service coordinator.
- Who signs? Provider and individual/LAR.
- Required before services? Yes.
- Needed attachments? Care plan, task list, medical notes.
- Updated when? When needs or provider change.
- Submitted to? The servicing agency/DSA records department.
- Used for? CLASS and CFC habilitation/PAS/HAB services.
- Legal basis? Texas service documentation requirements.
- Typical errors? Missing details and signatures.
Related Forms
- Service Delivery Plan (various CLASS program templates)
- Individual Plan of Care (IPC)
- Provider Agreement and Training Documentation
- Incident/Health and Safety Report Forms
Form Identification
- Name: Habilitation Service Provider Orientation / Supervisory Visits
- Form Number: 3599
- Region: State of Texas
- Program: CLASS / CFC
- Latest Revision: July 2015