TX HHS Form 3596. PAS/Habilitation Plan CLASS/DBMD/CFC
Form 3596 is a detailed service planning document used in Texas Medicaid waiver programs to define, authorize, and schedule Personal Assistance Services (PAS) and habilitation supports for individuals enrolled in CLASS, DBMD, and Community First Choice (CFC). The form translates an individual’s daily support needs into approved service hours, tasks, and weekly schedules that providers and caregivers must follow.
Purpose of Form 3596
The primary purpose of Form 3596 is to document exactly how PAS and habilitation services will be delivered to an individual. It establishes what assistance is needed, how often it will be provided, who delivers it, and how services align with the Individual Plan of Care (IPC).
This form serves as both an authorization and an operational guide. It ensures services are medically necessary, appropriately limited, and delivered consistently with Medicaid program rules.
When This Form Must Be Used
Form 3596 is required in the following situations:
- Initial enrollment into CLASS, DBMD, or CFC services
- Annual renewal of PAS or habilitation services
- Revisions due to changes in needs, schedules, or service delivery models
- Switching between Direct Services Agency (DSA) and Consumer Directed Services (CDS)
The form is not required for informal, unpaid caregiver support or services outside the approved Medicaid waiver.
Who Is Authorized to Complete the Form
Form 3596 is completed collaboratively by the program provider and the individual or their Legally Authorized Representative (LAR). Depending on the program, involvement may include:
- CLASS, DBMD, or CFC service providers
- Direct Services Agencies or CDS employers
- The individual receiving services or their LAR
- Service coordinators or case managers
All parties are responsible for ensuring the form accurately reflects approved services and does not exceed authorized limits.
Explanation of Key Sections
Individual and Program Information
This section identifies the individual, Medicaid number, IPC period, service delivery model, and enrollment status. Errors here can cause authorization or billing issues.
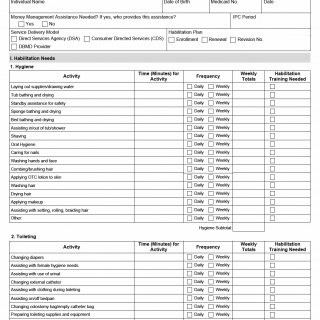
Habilitation Needs (Sections 1–14)
These sections break down daily living tasks into specific activities such as hygiene, toileting, dressing, meal preparation, feeding, exercise, transfers, cleaning, community assistance, supervision, and health-related tasks.
For each activity, the form records time, frequency, weekly totals, and whether habilitation training is required. This level of detail ensures services remain task-specific and compliant.
Habilitation Training
This section focuses on skill-building, such as money management, self-care, communication, community integration, and decision-making. It distinguishes training from routine assistance.
Weekly Schedule
The weekly schedule converts approved tasks into daily service hours. It defines when services occur and ensures weekly limits are not exceeded.
Non-Waiver Caregiver Support
This section documents unpaid support provided by family or caregivers. It helps clarify which supports are not Medicaid-funded and prevents duplication of services.
Service Totals and Agreements
Final sections summarize total authorized hours and costs and include acknowledgment statements confirming that schedules will not exceed approved limits.
Practical Tips for Completing Form 3596
- Base time estimates on realistic daily routines, not ideal scenarios.
- Ensure weekly totals match IPC-approved hours.
- Clearly separate habilitation training from routine assistance.
- Review caregiver support sections to avoid service overlap.
- Update schedules promptly when needs change.
Common Mistakes to Avoid
- Overestimating time for routine tasks
- Exceeding authorized weekly service limits
- Mixing unpaid caregiver support with waiver services
- Failing to revise the form after service changes
- Using vague descriptions instead of task-specific entries
Legal and Regulatory Context
Form 3596 is required under Texas Medicaid waiver rules governing CLASS, DBMD, and CFC programs. State regulations mandate precise documentation of PAS and habilitation services to ensure cost control, medical necessity, and accountability.
Improper or inaccurate completion may result in denied claims, recoupments, or compliance findings during audits.
Real-Life Examples of Use
- An individual’s PAS hours are increased after a change in mobility needs.
- A family switches from agency-provided services to CDS.
- A DBMD participant updates habilitation goals related to community integration.
- A schedule is revised due to a caregiver’s work schedule change.
Documents Commonly Used With This Form
- Individual Plan of Care (IPC)
- Service authorization notices
- Medical or functional assessments
- CDS employer agreements
- Provider service plans
Frequently Asked Questions
Does Form 3596 authorize new services?
No, it implements services already approved in the IPC.
Can schedules vary week to week?
Minor flexibility is allowed, but weekly limits cannot be exceeded.
Who signs or agrees to the schedule?
The individual or LAR and the service provider.
Is this form required for CDS?
Yes, it applies to both DSA and CDS delivery models.
What happens if hours are exceeded?
Exceeding limits may result in denied pa