TX HHS Form 3034. Provider Assessment Form
Form 3034, the Children with Special Health Care Needs (CSHCN) Provider Assessment Form, is a key medical evaluation document used in Texas to determine whether a child or qualifying individual meets the medical eligibility criteria for the CSHCN Services Program. This form is always completed by a licensed health care provider—not the applicant or parent—and it must accompany Form 3031 during initial application or renewal.
Purpose of Form 3034
This form helps the Texas Health and Human Services Commission (HHSC) verify that an applicant has a qualifying chronic physical condition or cystic fibrosis. It documents the severity of the condition, medical needs, diagnostic codes, and professional observations from the evaluating provider. Without this assessment, the applicant cannot be approved for CSHCN Services.
What This Form Actually Does
Form 3034 serves as an expert medical confirmation. HHSC uses it to understand:
- the primary and additional ICD-10 diagnoses, described at the highest specificity;
- the applicant’s functional limitations and long-term health outlook;
- whether delayed or unavailable treatment would worsen disability;
- the types of services the applicant may need beyond standard pediatric care.
Who Must Complete This Form
Only an evaluating provider who has examined the applicant within the last 12 months may complete and sign Form 3034. Eligible providers include:
- MD (Doctor of Medicine)
- DO (Doctor of Osteopathy)
- DDS or DMD (licensed dentists, when appropriate)
- APRN (Advanced Practice Registered Nurse)
- PA (Physician Assistant)
Mid-level practitioners must also list their supervising physician’s information.
When This Form Is Required
You must submit Form 3034 in the following cases:
- Initial application to the CSHCN Services Program
- Annual renewal of program eligibility
- When a child’s diagnosis or condition has significantly changed
- When HHSC requests updated medical documentation
It is not required when an applicant does not have a qualifying physical condition or when the provider has not evaluated the applicant in the past 12 months.
Key Sections of Form 3034 Explained
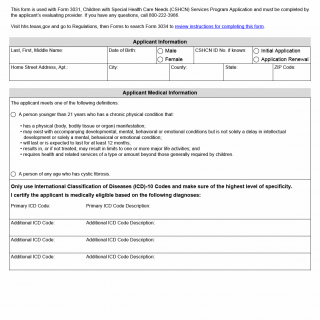
Applicant Information
This section identifies the applicant by name, date of birth, address, CSHCN ID number (if any), and whether the submission is for an initial application or a renewal. Providers should verify this information carefully, as mismatches frequently delay processing.
Medical Eligibility Criteria
The form specifies two qualifying conditions:
- A chronic physical condition lasting or expected to last at least 12 months, substantially limiting major life activities and requiring extensive health services.
- Cystic fibrosis, regardless of age.
Providers must certify the applicant meets one of these criteria.
ICD-10 Diagnostic Codes
Providers must list the primary diagnosis and any additional diagnoses using the most specific ICD-10 codes available. Broad or generic codes are a common mistake and often lead to requests for clarification.
Certification of Needs
This portion asks whether lack of care would cause permanent disability, pain, or death. Providers should include detailed notes on severity, complications, or treatment requirements. A brief statement like “complex condition” is insufficient.
Services That May Be Required
Providers can recommend non-medical or supportive services, such as:
- Case Management
- Home Health
- Mental Health Services
Birth and Trauma Information
This section applies mainly to infants and children with traumatic injuries. Providers should answer questions regarding premature birth, hospital stays, and accidents with specific dates.
Provider Information and Signature
The form must include:
- Provider’s full name and specialty
- NPI number
- Clinic address and phone
- Date of signature
The signature certifies that the provider personally evaluated the applicant.
Legislative and Administrative Background
The CSHCN Services Program is governed by Texas Health and Safety Code and overseen by the Texas Health and Human Services Commission. Form 3034 is mandatory because state regulations require verified medical eligibility from a licensed provider before public funds or medical support can be granted.
Practical Tips for Providers
- Ensure ICD-10 codes are precise and match the condition described.
- Provide clear statements about functional limitations, not just diagnoses.
- Confirm that the evaluation date is within 12 months of application.
- Avoid vague language—HHSC often requests clarification when descriptions lack detail.
- List all recommended services, even if the applicant is not currently receiving them.
Examples of Real Situations Where Form 3034 Is Needed
- A child with severe asthma who requires repeated hospitalizations and medication management beyond typical pediatric care.
- A teenager recovering from a spinal injury whose physical mobility limits daily activities and requires home health services.
- An infant born at 30 weeks with ongoing respiratory and developmental complications.
- An adult with cystic fibrosis seeking financial assistance for specialized treatments and equipment.
Documents Commonly Attached
- Recent medical records or discharge summaries
- Diagnostic test results (e.g., imaging, labs)
- Specialist reports supporting the diagnosis
- Therapy evaluations (PT/OT/SLP)
- Hospitalization timeline for premature infants
FAQ
- Who completes Form 3034? A licensed provider who evaluated the applicant in the last 12 months.
- Do parents or applicants fill out this form? No, only the medical provider completes and signs it.
- Is the form required for renewals? Yes, unless HHSC specifies otherwise.
- What happens if ICD-10 codes are vague? HHSC may delay processing and request additional documentation.
- Can a telehealth evaluation count? Yes, if the provider can adequately assess and document the condition.
- Where do I send the completed form? Return it to the applicant or mail it to the CSHCN Services Program Eligibility office in Austin.
- Does signing the form create liability? It certifies accuracy based on the provider’s knowledge but does not create new legal obligations.
Micro-FAQ (Short Answers)
- Purpose? Confirms medical eligibility for CSHCN services.
- Who completes? A licensed evaluating provider.
- Deadline? Required for application or annual renewal.
- Attachments? Medical records, ICD-10 documentation, discharge summaries.
- Submitted to? HHSC CSHCN Services Program.
- Who qualifies? Children with chronic physical conditions & individuals with cystic fibrosis.
- How often? Every 12 months.
- Evaluation needed? Yes, provider must have evaluated applicant within 12 months.
Related Forms
- Form 3031 – CSHCN Services Program Application
- Texas Medicaid Medical Necessity Forms
- Early Childhood Intervention (ECI) Medical Evaluation Forms
Form Summary
- Name: Children with Special Health Care Needs Provider Assessment Form
- Form Number: 3034
- Region: State of Texas
- Latest Revision: January 2025