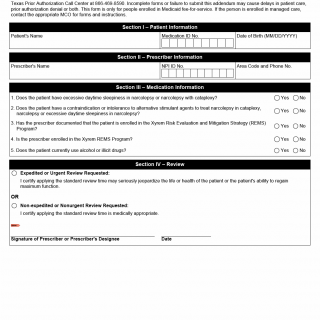
TX HHS Form 1356. Texas Medicaid Xyrem Prior Authorization Request
The Texas Medicaid Xyrem Prior Authorization Request Form (Form 1356) is a crucial document for healthcare providers to obtain approval for prescription medication benefits. This form helps solve the problem of ensuring that patients receive necessary treatment while streamlining the prior authorization process.
This standardized form requires prescribers to provide specific information about the patient, including their name, date of birth, and medication ID number. The form also includes questions about the patient's condition, such as excessive daytime sleepiness in narcolepsy or cataplexy, and any contraindications or intolerances to alternative stimulant agents. Additionally, prescribers must certify that the patient is enrolled in the Xyrem Risk Evaluation and Mitigation Strategy (REMS) Program, if applicable.
To complete this form, healthcare providers typically fax both Form 1356 and the Texas Standard Prior Authorization Request Form for Prescription Drug Benefits (TDI Form NOFRO02) to the Texas Prior Authorization Call Center at 866-469-8590. It is essential to submit a complete and accurate form to avoid delays in patient care or prior authorization denial. Key points to note include:
- Form completion is required for patients enrolled in Medicaid fee-for-service.
- Incomplete forms may cause delays or denial of prior authorization.
- Managed care enrollees should contact their MCO for forms and instructions.