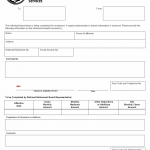
TX HHS Form 2710. Certification of Need for Major Dental Treatment
The Texas Health and Human Services (HHS) Form 2710, Certification of Need for Major Dental Treatment, is a crucial document that helps dentists certify the need for major dental treatment.
TX HHS Form 1026. Verification of Railroad Retirement Benefits
The TX HHS Form 1026, Verification of Railroad Retirement Benefits, is a crucial document that helps solve the problem of verifying retirement benefits received by individuals.
TX HHS Form 1025. Request for Information Medicare Advantage Coordination
Form 1025, titled Request for Information – Medicare Advantage Coordination, is an official Texas Health and Human Services Commission (HHSC) document used to verify community-based services received by an individual.
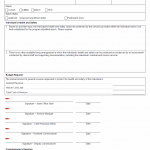
TX HHS Form 1024. Individual Status Summary
Form 1024, titled Individual Status Summary, is an official Texas Health and Human Services document used to justify situations where an individual’s services exceed established cost limits under certain Medicaid waiver programs.
TX HHS Form 1023. Request for Services Funded by General Revenue
The TX HHS Form 1023, Request for Services Funded by General Revenue, is a crucial document that helps solve the problem of ensuring the health and safety of individuals who require specialized services.
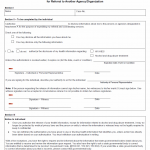
TX HHS Form 1022. Authorization to Disclose Information Including Protected Health Information for Referral to Another Agency/Organization
The TX HHS Form 1022 is a crucial document that enables individuals to authorize the disclosure of their health information for referral purposes.
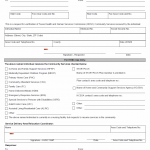
TX HHS Form 2705. Certification of Need for Major Medical Treatment
The TX HHS Form 2705, "Certification of Need for Major Medical Treatment", is a crucial document that helps healthcare professionals navigate the process of obtaining approval for major medical treatment or procedures.
TX HHS Form 2700. Application for a Treatment Decision by a Surrogate Consent Committee
The TX HHS Form 2700, Application for a Treatment Decision by a Surrogate Consent Committee, is a crucial document that helps solve the problem of obtaining treatment decisions for individuals with intellectual disabilities or related conditions.
TX HHS Form 2606. Managed Care Enrollment Processing Delay
The TX HHS Form 2606, Managed Care Enrollment Processing Delay, helps resolve processing delays in managed care enrollment for various programs, including Home and Community Based Services (HCBS) and Medically Dependent Children Program (MDCP).
TX HHS Form 2605. Member SK-SAI MDCP Review Signature
The TX HHS Form 2605, Member SK-SAI MDCP Review Signature, is a crucial document for reviewing the assessment results of the STAR Kids Screening and Assessment Instrument (SK-SAI).