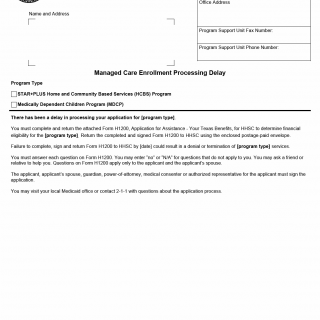
TX HHS Form 2606. Managed Care Enrollment Processing Delay
The TX HHS Form 2606, Managed Care Enrollment Processing Delay, helps resolve processing delays in managed care enrollment for various programs, including Home and Community Based Services (HCBS) and Medically Dependent Children Program (MDCP). This form is typically used by individuals who have experienced a delay in their application processing.
To complete the Form 2606, you must return the attached Form H1200, Application for Assistance - Your Texas Benefits, to HHSC using the enclosed postage-paid envelope. Failure to do so by the specified date may result in denial or termination of services. The form requires you to answer each question, with options to enter "no" or "N/A" for questions that don't apply. You can also seek assistance from a friend or relative.
Key points to note include:
- The Form H1200 must be completed and signed by the applicant, their spouse, guardian, power-of-attorney, medical consenter, or authorized representative.
- You can visit your local Medicaid office or contact 2-1-1 for questions about the application process.