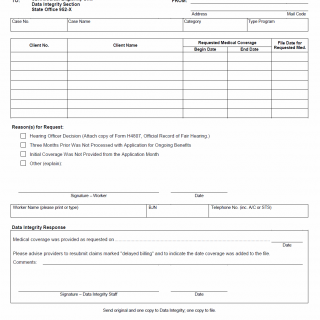
TX HHS Form H1107. Request for Forced Change of Medical Coverage
The TX HHS Form H1107, Request for Forced Change of Medical Coverage, is a crucial document that helps resolve issues with medical coverage. This form is typically used in situations where a client's medical coverage needs to be changed due to various reasons such as hearing officer decisions or delayed billing.
This form requires specific information from the worker, including the requested medical coverage file date for the client, the reason(s) for the request, and the signature of the worker. The Data Integrity Section is responsible for processing the request and providing medical coverage as requested. If there are any issues with claims marked "delayed billing", providers are instructed to resubmit them.
Key features of this form include the requirement to attach a copy of Form H4807, Official Record of Fair Hearing, in cases where a hearing officer decision is involved. The Data Integrity Staff is responsible for sending the original and one copy to their office, with another copy going to the file. By using this form, workers can ensure that medical coverage changes are processed efficiently and effectively.
- This form is used when there is a need to change a client's medical coverage due to various reasons such as hearing officer decisions or delayed billing.
- The worker must provide specific information including the requested medical coverage file date, reason(s) for the request, and signature.
- Providers are instructed to resubmit claims marked "delayed billing" and indicate the date coverage was added to the file.