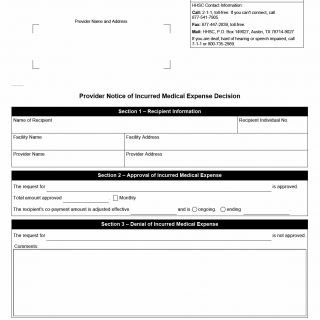
TX HHS Form H1053-IME. Provider Notice of Incurred Medical Expense Decision
The Provider Notice of Incurred Medical Expense Decision (Form H1053-IME) is a communication tool used by the Texas Health and Human Services Commission (HHSC). It informs long-term care providers about HHSC’s decision to approve or deny an individual's Incurred Medical Expense (IME). Providers receive this form when a resident of a Medicaid-certified facility has requested an adjustment to their co-payment based on qualifying medical costs.
Purpose and Importance of the Form
This document is essential because it directly affects how much a Medicaid recipient must contribute toward their cost of care each month. IME adjustments can lower the resident’s monthly co-payment, allowing the facility to bill Medicaid for a greater share of the cost. HHSC uses this form to provide an official, trackable decision that providers must follow.
Texas Medicaid rules require HHSC to notify facilities in writing when an IME request has been reviewed. This protects both residents and providers by ensuring that any change to co-payment amounts is properly authorized and documented.
Explanation of Each Section of the Form
Section 1 – Recipient Information
This section identifies the Medicaid recipient whose IME request was evaluated. It includes:
- Name of Recipient – Must match Medicaid records.
- Recipient Individual Number – The unique Medicaid ID.
- Facility Name and Address – The nursing facility or group home providing long-term care.
- Provider Name and Address – Usually the billing or administrative entity.
Typical mistake: Providers sometimes mismatch facility and corporate provider addresses. This can delay HHSC communications.
Section 2 – Approval of Incurred Medical Expense
This section appears when HHSC approves the IME request. It states:
- What medical expense was approved
- The total approved amount
- Whether it applies monthly or as a one-time adjustment
- The effective date when the adjusted co-payment begins
- Whether the adjustment is ongoing or ends on a specific date
Why it matters: The co-payment is the amount the resident must contribute from their income; when this amount is reduced, the facility’s claim to Medicaid increases correspondingly.
Section 3 – Denial of Incurred Medical Expense
If HHSC denies the request, this section will appear instead. It specifies the item or expense that was not approved and includes a comments field explaining the reason. Reasons may include:
- The expense is not allowable under Medicaid rules
- Insufficient documentation
- The service was not medically necessary
- The cost was already reimbursed by another party
Important confidentiality note: HHSC does not disclose final co-payment amounts to providers unless the resident or their authorized representative gives written permission.
Legislative and Regulatory Background
IME decisions are governed by Texas Medicaid policy for long-term care services, which allows recipients to request deductions from income for certain medical expenses not covered by Medicaid. This ensures fairness for individuals who must pay out-of-pocket for medically necessary services.
Practical Advice for Providers
- Ensure the facility’s administrative address is correct; incorrect contact data is a common cause of delays.
- When submitting IME documentation to HHSC, include itemized receipts, dates of service, and proof of payment.
- If the resident has an authorized representative, obtain written consent early to avoid communication barriers.
- Track effective dates carefully—an IME approval may retroactively change billing periods.
Examples of Real-Life Situations
- A resident purchases necessary dental services not covered by Medicaid, submitting receipts for an income deduction.
- A nursing home resident requires specialized foot care from a podiatrist and pays out-of-pocket; HHSC later approves the expense.
- A family hires a private medical transport service for a resident’s hospital visit; HHSC denies it because Medicaid transportation was available.
- A resident purchases durable medical equipment not included in their Medicaid benefit plan; the expense is partially approved.
Documents Commonly Attached to an IME Request
- Itemized medical bills
- Receipts showing proof of payment
- Physician statements of medical necessity
- Insurance denial letters (if applicable)
- Service provider invoices
FAQ
- What is an Incurred Medical Expense?
It is a medical cost paid out-of-pocket by a Medicaid recipient that may reduce their required co-payment. - Can a facility submit an IME request on behalf of a resident?
Yes, but proper authorization from the resident or representative must be on file. - How long does HHSC take to review IME requests?
Processing times vary, but providers generally receive Form H1053-IME once a decision is finalized. - Why might an IME be denied?
Common reasons include incomplete documentation, unallowable expenses, or services not considered medically necessary. - Does an IME approval change past billing?
It may; some adjustments are retroactive depending on the effective date shown on the form. - Can providers see the resident’s final co-payment?
Only with written authorization from the resident or their representative.
Micro-FAQ
- Purpose: Notify providers of HHSC’s decision on a resident’s medical expense deduction.
- Who files: Residents, representatives, or facility staff with authorization.
- Effective date: Shown in Section 2 for approvals.
- Attachments: Receipts, invoices, medical necessity notes.
- Submitted to: Texas HHSC via 2-1-1, fax, or mail.
- Denial reasons: Non-allowable costs, missing paperwork, not medically necessary.
- Confidentiality: Providers cannot receive co-payment amounts without permission.
- Applies to: Medicaid long-term care residents in Texas.
Related Forms
- Form H1053 – Notice of Action
- Form H1746-A – MEPD Referral Cover Sheet
- Form H1200 – Application for Assistance (Texas Medicaid)
- Form H1020 – Request for Information
Form Details (Official Identification)
- Form Name: Provider Notice of Incurred Medical Expense Decision
- Form Number: H1053-IME
- Agency: Texas Health and Human Services Commission (HHSC)
- Region: Texas
- Date of Edition: 09/2025