TX HHS Form 8511. Understanding Program Eligibility and Services
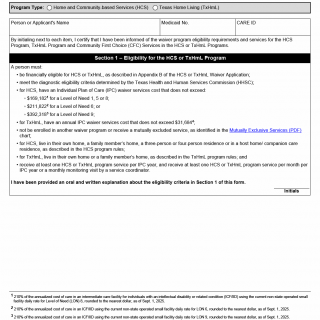
Form 8511 is used in Texas to help individuals and families understand the eligibility rules and core service principles for the Home and Community-based Services (HCS) Program and the Texas Home Living (TxHmL) Program. These programs support people with intellectual disabilities or related conditions, allowing them to receive care in community settings instead of institutional facilities. This form is typically reviewed with the applicant during the eligibility process and requires initials to confirm that all information has been explained and understood.
Purpose of Form 8511
The form ensures that the applicant (or their legally authorized representative) acknowledges key program eligibility requirements, living arrangement rules, cost limits, and other conditions set by the Texas Health and Human Services Commission (HHSC). Although the form itself does not determine eligibility, it documents that the applicant understands what the programs require and what services may be provided.
Overview of Eligibility Requirements
Eligibility for the HCS and TxHmL programs is determined by several state-defined criteria. Form 8511 summarizes these criteria, which include financial qualifications, diagnostic confirmation, annual cost limits, and residency rules. Below is a clearer breakdown of each item.
Financial Eligibility
Applicants must meet financial requirements described in Appendix B of the official HCS or TxHmL Waiver Application. These financial guidelines determine whether the applicant qualifies for Medicaid-funded waiver services.
Diagnostic Eligibility
The applicant must meet the diagnostic criteria defined by HHSC, typically involving documentation of an intellectual disability or related condition. Assessments are performed or verified through authorized professionals.
Cost Limits for HCS and TxHmL
Each program has annual cost caps that cannot be exceeded by the Individual Plan of Care (IPC):
- For HCS:
- LON 1, 5, or 8: $169,182
- LON 6: $211,822
- LON 9: $392,318
- For TxHmL: $31,684 annually
These limits ensure the services provided at home do not exceed the projected cost of comparable services in an intermediate care facility.
Mutually Exclusive Services
Applicants cannot receive services from conflicting Medicaid waiver programs at the same time. The HHSC Mutually Exclusive Services chart lists combinations that are not allowed.
Required Living Arrangement
- HCS: The applicant may live in their own home, a family member’s home, a three- or four-person residence, or a host home/companion care setting.
- TxHmL: The applicant must live in their own home or a family member’s home.
Service Participation Requirements
To remain active in the program, the applicant must receive at least one service per IPC year and at least one service or a monitoring visit each month.
Common Mistakes Applicants Make
- Not understanding that exceeding IPC cost limits may delay or prevent eligibility.
- Attempting to enroll in another waiver program at the same time, which the rules prohibit.
- Submitting outdated diagnostic documentation without proper verification.
- Failing to maintain the required living arrangement described in program rules.
When You Should and Should Not Submit This Form
- Submit: When beginning the HCS or TxHmL enrollment process, typically during the eligibility review.
- Do Not Submit: If evaluating options but not yet pursuing HCS or TxHmL, or if you are already active in another Medicaid waiver that cannot be combined.
Who May Complete the Form
- The applicant (if capable of providing informed acknowledgment)
- A legally authorized representative (LAR), including:
- parent of a minor
- court-appointed guardian
- authorized agent under a valid power of attorney, where applicable
Documents Commonly Attached or Reviewed
- Medicaid eligibility records
- Diagnostic assessments verifying intellectual disability or related condition
- Care plans or evaluations used to determine the Level of Need
- Proof of residence and living arrangement
Legal and Practical Consequences of This Form
By initialing the sections of Form 8511, the applicant confirms that program rules were fully explained. While the form does not itself approve or deny services, it becomes part of the permanent eligibility file. Misunderstanding or misrepresenting information on this form can delay service authorization or lead to administrative complications.
Practical Tips for Completing Form 8511
- Initial each item only after the explanation is fully understood.
- Ask the service coordinator to clarify any unfamiliar terms, especially cost limits and LON categories.
- Keep a copy of the completed form for your personal records.
- Make sure diagnostic documents are up to date and signed by authorized professionals.
- Confirm that you meet the required living arrangement before signing.
Real-Life Situations Where This Form Is Needed
- Scenario 1: A family caring for an adult son with an intellectual disability applies for HCS services to move him into a supported host home.
- Scenario 2: A grandmother is the legal representative for her minor grandson and needs TxHmL services to support him while he continues living at home.
- Scenario 3: An individual transitioning out of an institutional care facility needs waiver services and must document understanding of eligibility rules.
- Scenario 4: A legal guardian begins the enrollment process after the applicant receives a new Level of Need assessment that qualifies for HCS funding.
FAQ
- Is Form 8511 an application for services? No. It confirms understanding of eligibility criteria but does not enroll you in a program.
- Do I need to submit proof of diagnosis with this form? Documentation is reviewed during eligibility determination, but this form only records acknowledgment.
- Can I receive HCS and another Medicaid waiver at the same time? No. Certain services are mutually exclusive according to HHSC rules.
- What happens if my IPC exceeds the cost limit? The plan must be adjusted before approval; otherwise, eligibility may be denied.
- Who signs if the applicant cannot? A legally authorized representative may sign and initial the form.
- Do I need to complete this form every year? It is typically completed during the enrollment or renewal process when required by the program coordinator.
- Does initialing this form obligate me to enroll? No. It only acknowledges that information was provided.
Micro-FAQ (Short Answers)
- Purpose? Acknowledging HCS/TxHmL eligibility rules.
- Who completes it? Applicant or legal representative.
- Submitted to? Service coordinator or program provider.
- Attachments? None required, but diagnostic records are reviewed separately.
- Is it mandatory? Yes, during the eligibility explanation process.
- Used for? Documenting informed understanding.
- Renewed? As requested during eligibility updates.
- Part of Medicaid? Yes, for waiver programs.
- Cost limits included? Yes, by LON category.
- Does it approve services? No.
Related Forms
- HCS Program Consumer Information Form
- TxHmL Service Plan Template
- Community First Choice (CFC) Services Acknowledgment
- HHSC Diagnostic Assessment Documentation
Form Details
- Form Name: Understanding Program Eligibility and Services
- Form Number: 8511
- Program: Home and Community-based Services (HCS), Texas Home Living (TxHmL)
- Region: State of Texas
- Edition Date: September 2025