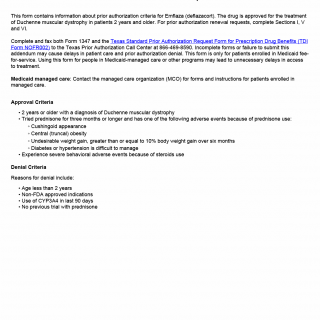
TX HHS Form 1347. Emflaza Prior Authorization Request
The TX HHS Form 1347, Emflaza Prior Authorization Request, is a crucial document that helps healthcare providers obtain prior authorization for the treatment of Duchenne muscular dystrophy patients with Emflaza (deflazacort). This form is used in situations where patients require ongoing treatment and need to demonstrate that they meet specific criteria for continued therapy.
The form requires completion of Sections I, V, and VI, which involve providing information about patient diagnosis, previous treatment attempts, and adverse events. Healthcare providers must also ensure that the patient meets the approval criteria, including being at least 2 years old with a confirmed diagnosis of Duchenne muscular dystrophy and having tried prednisone for three months or longer without satisfactory results.
Key features of this form include the need to complete both Form 1347 and the Texas Standard Prior Authorization Request Form for Prescription Drug Benefits (TDI Form NOFROO2) and fax them to the Texas Prior Authorization Call Center. Failure to submit a complete form may result in delays or denial of prior authorization. It is essential to note that this form is only applicable for patients enrolled in Medicaid fee-for-service, and healthcare providers should contact managed care organizations (MCOs) for forms and instructions if treating patients in Medicaid-managed care programs.
- This form is used for patients with Duchenne muscular dystrophy who require Emflaza treatment.
- Healthcare providers must complete Sections I, V, and VI to demonstrate patient eligibility.
- The form requires faxing both Form 1347 and the Texas Standard Prior Authorization Request Form for Prescription Drug Benefits (TDI Form NOFROO2) to the Texas Prior Authorization Call Center.