Prior Authorization Form
A Prior Authorization form is a document that healthcare providers use to request approval from an insurance company or other payer to cover a specific medical treatment or service. The primary purpose of the form is to ensure that patients receive the necessary medical care while also controlling healthcare costs.
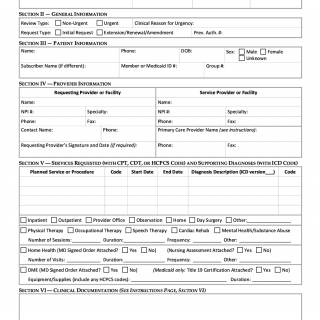
The form consists of several essential sections, including the patient's name, date of birth, and insurance information. It also includes the provider's name and contact information, a description of the requested treatment or service, and the reason for the request. Additionally, the form may require supporting documentation, such as medical records or test results.
The parties involved in the prior authorization process include the healthcare provider, the insurance company or other payer, and the patient. It is important to consider the specific requirements of the insurance plan and the potential risks and benefits of the requested treatment or service before completing the form.
When compiling the prior authorization form, healthcare providers will need to provide the patient's personal and insurance information, as well as a detailed description of the requested treatment or service. Supporting documentation, such as medical records or test results, may also be required.
Application examples and use cases of the prior authorization form include requesting approval for a specific medication or medical procedure, such as surgery or diagnostic imaging. Strengths of the form include ensuring that patients receive necessary medical care while controlling healthcare costs, while weaknesses include potential delays in receiving approval and denials of coverage.
Alternative forms to the prior authorization form include the pre-certification form and the pre-authorization form. These forms differ in the specific requirements and parties involved in the approval process.
The prior authorization form can significantly impact the future of the patient, as it determines whether insurance will cover the requested treatment or service. The form is typically submitted to the insurance company or other payer for review and is stored in the patient's medical records.
In summary, the prior authorization form is a critical document that healthcare providers use to request approval from insurance companies or other payers to cover specific medical treatments or services. It consists of essential sections and may require supporting documentation. It has various applications and use cases, strengths, weaknesses, and alternative forms. The form can significantly impact the future of the patient and is typically submitted to the insurance company or other payer for review.