Humira Appeal Letter
A Humira appeal letter is a formal written communication submitted to a healthcare insurance provider, pharmaceutical assistance program, or relevant authority. Its purpose is to contest the denial or restriction of coverage for the medication Humira (adalimumab), which is used to treat autoimmune conditions such as rheumatoid arthritis, psoriasis, Crohn's disease, and ulcerative colitis. The appeal letter presents a compelling case to persuade the recipient to reconsider their decision by providing detailed medical justifications, supporting evidence, and a clear argument for the medical necessity of Humira.
How to Perform a Humira Appeal Letter:
1. Gather Information: Collect all relevant medical records, diagnostic reports, treatment history, and correspondence related to the denied coverage of Humira. This documentation will serve as the backbone of your appeal.
2. Understand Denial Reasons: Carefully review the denial letter you received. Understand the specific reasons for the denial, such as cost concerns, lack of medical necessity documentation, or failure to meet certain criteria. This understanding will guide your approach in crafting the appeal.
3. Research Medical Guidelines: Consult medical guidelines relevant to your condition, such as those provided by reputable medical associations or institutions. Highlight how Humira aligns with these guidelines and how it can address your specific medical needs.
4. Craft the Appeal Letter: Structure your appeal letter in a professional and organized manner. Include the following components:
-
Header: Include your contact information, date, and recipient's details.
-
Introduction: State your purpose clearly and concisely. Mention the denial decision and reference the date and reference number from the denial letter.
-
Patient's Information: Provide the patient's name, age, medical condition, and a brief overview of their medical history.
-
Medical Justification: Detail the severity of the patient's condition, the impact it has on their daily life, and how previous treatments have been inadequate. Reference specific symptoms, limitations, and challenges they face.
-
Relevance of Humira: Explain why Humira is the recommended treatment. Highlight its efficacy, safety profile, and the potential benefits for the patient. Reference medical guidelines or expert opinions that support its use.
-
Documentation: Attach all relevant medical records, test results, treatment history, and any letter of medical necessity provided by the prescribing physician.
-
Request for Reconsideration: Clearly state that you are appealing the denial decision and provide a well-reasoned argument for why Humira coverage should be approved. Address the specific reasons for denial and provide counterpoints supported by evidence.
-
Contact Information: Provide your contact information and invite the recipient to reach out for further clarification or additional information.
-
Closing: Thank the recipient for their attention and consideration. Express hope for a positive resolution.
5. Review and Edit: Proofread the appeal letter for clarity, accuracy, and professionalism. Ensure that all relevant information is included and that the language is persuasive and respectful.
6. Submit the Appeal: Submit the appeal letter according to the instructions provided in the denial letter. This may involve mailing a physical copy, uploading it to an online portal, or sending it via email.
7. Follow Up: After submitting the appeal, follow up with the recipient to confirm receipt and inquire about the expected timeline for a response. Be prepared to provide any additional information or documentation they may request.
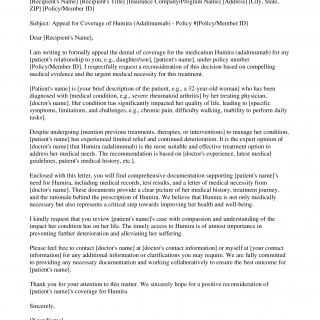
Sample of Humira Appeal Letter
[Your Name] [Your Address] [City, State, ZIP] [Your Phone Number] [Your Email Address] [Date]
[Recipient's Name] [Recipient's Title] [Insurance Company/Program Name] [Address] [City, State, ZIP] [Policy/Member ID]
Subject: Appeal for Coverage of Humira (Adalimumab) - Policy #[Policy/Member ID]
Dear [Recipient's Name],
I am writing to formally appeal the denial of coverage for the medication Humira (adalimumab) for my [patient's relationship to you, e.g., daughter/son], [patient's name], under policy number [Policy/Member ID]. I respectfully request a reconsideration of this decision based on compelling medical evidence and the urgent medical necessity for this treatment.
[Patient's name] is [your brief description of the patient, e.g., a 32-year-old woman] who has been diagnosed with [medical condition, e.g., severe rheumatoid arthritis] by her treating physician, [doctor's name]. Her condition has significantly impacted her quality of life, leading to [specific symptoms, limitations, and challenges, e.g., chronic pain, difficulty walking, inability to perform daily tasks].
Despite undergoing [mention previous treatments, therapies, or interventions] to manage her condition, [patient's name] has experienced limited relief and continued deterioration. It is the expert opinion of [doctor's name] that Humira (adalimumab) is the most suitable and effective treatment option to address her medical needs. The recommendation is based on [doctor's experience, latest medical guidelines, patient's medical history, etc.].
Enclosed with this letter, you will find comprehensive documentation supporting [patient's name]'s need for Humira, including medical records, test results, and a letter of medical necessity from [doctor's name]. These documents provide a clear picture of her medical history, treatment journey, and the rationale behind the prescription of Humira. We believe that Humira is not only medically necessary but also represents a critical step towards improving her health and well-being.
I kindly request that you review [patient's name]'s case with compassion and understanding of the impact her condition has on her life. The timely access to Humira is of utmost importance in preventing further deterioration and alleviating her suffering.
Please feel free to contact [doctor's name] at [doctor's contact information] or myself at [your contact information] for any additional information or clarifications you may require. We are fully committed to providing any necessary documentation and working collaboratively to ensure the best outcome for [patient's name].
Thank you for your attention to this matter. We sincerely hope for a positive reconsideration of [patient's name]'s coverage for Humira.
Sincerely,
[Your Name]
[Your Title/Position]
[Your Contact Information]