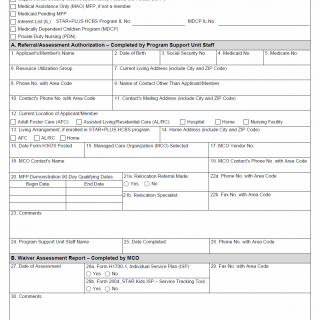
TX HHS Form H3676. Managed Care Pre-Enrollment Assessment Authorization
Form H3676, titled "Managed Care Pre-Enrollment Assessment Authorization," is used within Texas Medicaid programs to authorize and document pre-enrollment assessments for individuals participating in various managed care and waiver programs. This form ensures that applicants meet program criteria and that all necessary data is collected before enrollment or service provision.
Purpose of Form H3676
The form is designed to streamline pre-enrollment for multiple Medicaid programs including STAR+PLUS HCBS, Medical Assistance Only (MAO) MFP, Medically Dependent Children Program (MDCP), Private Duty Nursing (PDN), and other related initiatives. It ensures accurate documentation of applicant information, living arrangements, MCO selection, and program eligibility. Submitting this form helps facilitate timely enrollment and service delivery while maintaining compliance with state regulations.
Section-by-Section Explanation
A. Referral/Assessment Authorization – Program Support Unit Staff
- Applicant’s/Member’s Information: Captures personal identifiers including name, date of birth, Social Security number, Medicaid and Medicare numbers. Common mistake: entering incorrect identifiers can delay processing.
- Contact Information: Current address, phone number, and an alternate contact. Tip: Ensure all phone numbers include area codes and are current.
- Living Arrangement: Details the type of residence (AFC, AL/RC, Home, Hospital, Home Nursing Facility). Helps MCO staff determine appropriate services.
- MCO Selection: Name and contact of the Managed Care Organization, including vendor number. Correct entry ensures services are coordinated with the proper organization.
- MFP Demonstration Dates: Begin and end dates for Money Follows the Person eligibility. Must match program records to validate participation.
- Relocation Referral: Indicates whether a referral was made and identifies the relocation specialist. Common errors include missing dates or specialist names.
- Program Support Unit Staff Completion: Staff member signs, dates, and provides contact info to verify authorization.
B. Waiver Assessment Report – MCO Staff
- Date of Assessment: Records the day the waiver assessment was conducted.
- Individual Service Plans: References Form H1700-1 or Form 2604 (STAR Kids ISP). Confirms that an appropriate plan is in place.
- Medical Necessity Approval: Indicates whether the individual qualifies medically for services.
- Community First Choice Eligibility: Confirms eligibility for CFC-only services.
- MFP Participation: Verifies participant inclusion in the Money Follows the Person demonstration.
- MCO Staff Completion: Staff member records name, date, and contact info to validate the assessment.
Practical Recommendations
- Ensure all personal identifiers are accurate to prevent delays.
- Double-check contact numbers and addresses for applicants and alternate contacts.
- Provide full documentation for living arrangements and program eligibility.
- Include all required supporting forms (ISP, service tracking tools) with submission.
- Confirm dates for MFP demonstration and relocation referrals match official records.
Examples of Real-Life Use
- An adult Medicaid recipient moving from institutional care to a home-based care program submits Form H3676 to document eligibility and coordinate with the selected MCO.
- A child with medically complex needs is enrolling in the MDCP program; the MCO uses the form to complete the waiver assessment and confirm service planning.
- A participant transitioning from MAO MFP to a STAR+PLUS HCBS program uses the form to verify relocation dates and program eligibility.
Documents Typically Required
- Individual Service Plan (ISP) – Form H1700-1
- STAR Kids Service Tracking Tool – Form 2604
- Medical documentation supporting eligibility
- Proof of current living arrangement (lease, hospital discharge summary, etc.)
Frequently Asked Questions
Who must complete Form H3676?
The Program Support Unit staff and the Managed Care Organization (MCO) personnel responsible for pre-enrollment assessments.
When is this form required?
Required for all applicants enrolling in Medicaid waiver programs, MFP initiatives, or managed care pre-enrollment processes.
Can family members submit the form?
Only authorized MCO or Program Support Unit staff can complete and submit the form.
What common mistakes should be avoided?
- Incorrect personal identifiers (SSN, Medicaid number)
- Missing MCO contact information
- Incomplete dates for MFP participation or relocation referrals
What supporting documents are necessary?
ISP, service tracking forms, medical documentation, and proof of current living arrangement.
What happens after submission?
The MCO reviews the form, completes the waiver assessment, approves medical necessity, and records participation in applicable programs.
Micro-FAQ (Quick Answers)
- Purpose: Authorize and document pre-enrollment assessments for Medicaid programs.
- Who files: Program Support Unit and MCO staff.
- Deadline: Must be completed before enrollment or service initiation.
- Attachments: ISP, service tracking forms, medical documents.
- Submitted to: Managed Care Organization and Program Support Unit.
- Eligibility check: Confirms program eligibility and living arrangements.
- Medical necessity: Determines approval for services.
- MFP dates: Must match official records for Money Follows the Person program.
Related Forms
- Form H1700-1 – Individual Service Plan (ISP)
- Form 2604 – STAR Kids Service Tracking Tool
- Form H3675 – Managed Care Enrollment
- Form H1600 – MFP Program Documentation
Form Details
- Form Name: Managed Care Pre-Enrollment Assessment Authorization
- Form Number: H3676
- Region: Texas
- Revision Date: September 2017-E