TX HHS Form 8584-CDS. Comprehensive Nursing Assessment and Plan of Care HCS Program
Form 8584-CDS is a comprehensive nursing assessment and plan of care used in the Consumer Directed Services (CDS) option of the Home and Community-based Services (HCS) program. A Registered Nurse (RN) performs the assessment to document medical history, current status, nursing needs, and to determine safe medication and task delegation for individuals receiving CDS.
Purpose of Form 8584-CDS
The form documents a full nursing review used to:
- Assess current medical, psychiatric and functional status.
- Review medications, allergies and adverse reactions.
- Perform systems-based examinations and vital signs.
- Evaluate behavioral, communication and pain presentation.
- Decide on RN delegation or need for licensed nursing care.
- Create a nursing plan of care with interventions, goals and monitoring schedule.
Who Completes This Form
The assessment and plan are completed and signed by a Registered Nurse (RN). The RN documents consultations, coordinates with the individual’s health care team, and records physician involvement. The individual, CRA/LAR, or Provider Advocate Committee (PAC) may participate in decision sections as applicable.
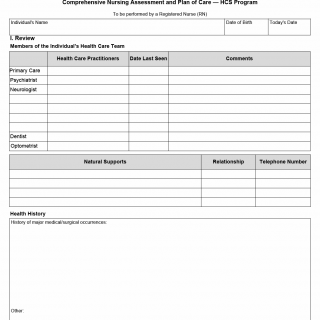
Section I — Review and Health Care Team
RN documents members of the individual’s health care team (PCP, psychiatrist, neurologist, dentist, optometrist, natural supports), last seen dates and relevant comments. This section also includes a comprehensive medication review (including OTCs, vitamins, herbs), allergies, doses, routes, purposes, side effects and required labs.
Section II — Current Status and Vitals
RN summarizes recent changes (hospitalizations, falls, seizures, restraints), records vital signs (BP, pulse, respirations, temperature, pain, weight, height) and identifies primary concerns from the individual/CRA perspective. Fall risk assessment and cause (neurological, musculoskeletal, unknown) are noted.
Section III — Review of Systems
Systematic review covering:
- Neurological (seizure type/frequency, tremors, balance, paralysis)
- Eyes/Ears/Nose/Throat (vision, hearing, swallowing)
- Cardiovascular (edema, chest pain, BP abnormalities)
- Gastrointestinal (feeding tube, bowel program, reflux, vomiting)
- Respiratory (wheezing, oxygen, aspiration history)
- Musculoskeletal (pain, contractures, gait impairment)
- Genitourinary (UTI history, incontinence, bladder program)
- Integumentary (skin integrity, wounds, breakdown risk)
- Endocrine (diabetes, blood sugar management)
Section IV — Additional Health Status
Includes immunizations, nutritional assessment (route of nutrition, therapeutic diet, swallowing concerns), sleep patterns, activity level, substance use, and weight changes. RN documents assistive devices, dietary needs and interactions with medications.
Mental Status and Behavior
RN records appearance, cognition, memory/orientation, mood, thought content (delusions/hallucinations), communication methods, challenging behaviors, frequency and severity scales, and whether medications or formal behavior plans are in place.
Pain and Communication
Assessment of how pain is expressed (verbal, facial, body language, augmented devices), ability to use a pain scale and any adaptive communication devices used by the individual.
Section V — Implementation Assessment (Decision Making & Supports)
RN evaluates health care decision-making capacity (full, limited, or unable), documents support system adequacy (CRA/parent, host home, guardian, PAC), and determines need and frequency of RN reassessment. Knowledge and demonstrated technique for key health tasks are recorded for the individual and CRA.
Delegation and Safe Administration of Medications
RN determines whether medication administration or health maintenance activities (HMAs) may be self-administered, safely directed by a CRA, or require RN delegation. The form clarifies which routes/tasks may be delegated to paid unlicensed personnel, supervision level, competency verification, and follow-up schedule (initial, monthly, quarterly, etc.).
RN Supervision and Nurse Follow-up
RN specifies names of unlicensed personnel, members consulted to set supervision level, frequency of RN monitoring, and additional LVN or RN oversight required to ensure competency and safety.
Section VI — Plan of Care / Summary
RN provides a clinical summary and nursing service plan documenting:
- Clinical impressions and recommended consultations
- Nursing diagnoses/concerns and strengths
- Interventions, implementation strategies, objectives, start and target completion dates
- Calculation of nursing units and total nursing units needed
- Desired outcomes/goals and responsible clinician signatures (RN and physician)
Documentation and Accountability
The RN signs and retains accountability for the plan, ensures competency verification before delegated tasks are performed unsupervised, and documents immediate phone accessibility for unlicensed personnel when tasks are performed.
Who Uses Form 8584-CDS
- Registered Nurses conducting CDS assessments for HCS participants
- CDS employers, unlicensed assistive personnel and CRAs/LARs
- Physicians and interdisciplinary teams coordinating care
- Program auditors and case managers reviewing nursing plans
Why This Form Is Important
- Ensures safe medication practices and appropriate delegation decisions.
- Documents comprehensive health and behavioral needs to guide care.
- Defines RN oversight and monitoring to protect individual safety.
- Forms the basis for individualized nursing interventions and service allocation.
Key Form Details
- Form: 8584-CDS
- Title: Comprehensive Nursing Assessment and Plan of Care — CDS Option (HCS Program)
- Issued: August 2014
- Completed by: Registered Nurse (RN)