TX HHS Form 7239. Incident or Illness Report
Form 7239 is used by Texas child-care operations to document injuries, the onset of illnesses, and reportable incidents involving a child. While the form may look straightforward, it plays a central role in regulatory compliance, parent communication, and documenting events that may have legal or medical consequences. This guide explains each section in practical terms so staff can complete it accurately and confidently.
Purpose of Form 7239
This form is required under Texas Health and Human Services (HHSC) minimum standards. It ensures that every significant injury, illness requiring medical evaluation, or communicable disease event is formally recorded. The document becomes part of the operation’s official record and must be provided to parents and, in certain cases, regulatory authorities. Properly completing this form protects both the child and the operation, providing a transparent account of what happened and how staff responded.
When You Must Use This Form
- When a child sustains an injury needing medical treatment or hospitalization.
- When an incident occurs that places a child at risk of harm (even if no injury resulted).
- When a child becomes ill and requires hospitalization.
- When a child or staff member contracts a communicable disease that must be reported.
You do not need this form for everyday bumps, minor scrapes, or mild symptoms that do not require medical care—unless your internal policies require it.
Who Is Allowed to Complete the Form
The form must be completed by the director, caregiver in charge, or another staff member designated by the operation. Final review and certification must always be done by the director or person in charge (Section V).
Overview of Key Sections
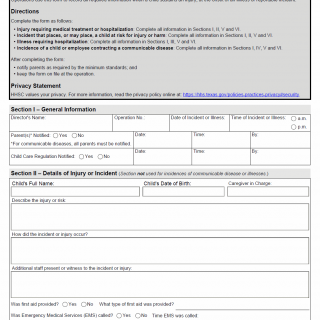
Section I – General Information
This section establishes the basic facts: when the incident occurred, who was present, and when parents and Child Care Regulation (CCR) were notified. It also documents whether all parents were notified in cases involving communicable diseases, as required by Texas rules.
- Common mistake: forgetting to record the time parents were notified—this is a compliance requirement.
- Tip: record the notification method (call, email, in person) even if not explicitly required.
Section II – Details of Injury or Incident
This section is only for accidents or non-medical incidents. You must describe:
- What happened and how it happened
- Who witnessed the event
- What first aid was provided
- Whether EMS was called
- Whether the child was transported for medical care
Descriptions must be factual, without assumptions or blame. Avoid language like "the child wasn't paying attention"—instead describe observable actions.
Section III – Illness Requiring Hospitalization
This section is used when a child becomes ill and the illness requires emergency medical attention or hospitalization. Required information includes:
- Symptoms, fever readings, and timeline
- Medication given at the operation
- EMS involvement
- Communication with the child’s doctor
- Allergy plans or epinephrine use, if applicable
Accuracy here is especially important because this documentation may later be reviewed by medical providers or investigators.
Section IV – Communicable Disease
Use this section when a child or employee contracts a communicable disease that must be reported or shared with parents. You must record:
- Type of disease
- Whether exclusion is required
- Whether the Health Department was notified
Texas rules require notifying all parents when communicable diseases pose risks to the group environment.
Section V – Employee or Caregiver Certification
The director or person in charge certifies that the information is accurate and complete. Incomplete or unsigned forms are considered non-compliant documentation.
Section VI – Parent or Guardian Acknowledgment
Parents sign to confirm they received the information. If sent electronically, attach proof (email timestamp or message screenshot).
Practical Tips for Completing the Form
- Write clearly and avoid abbreviations that parents may not understand.
- Record times as accurately as possible—use center logs if needed.
- Describe injuries and incidents factually, focusing on observable details.
- If unsure whether EMS must be called, document your decision-making process.
- Attach supporting notes if space on the form is insufficient.
Common Mistakes to Avoid
- Leaving blank fields instead of writing “N/A.”
- Failing to notify parents in communicable disease cases.
- Using vague statements like “child got hurt”—be specific.
- Recording opinions instead of events.
Examples of Real-Life Situations
- Playground Injury: A child falls from a low climbing structure and appears disoriented. First aid is provided, and the child is taken for medical evaluation. Form 7239 documents the sequence of events and parental notification.
- Sudden Fever: A child develops a 103°F fever during nap time. Staff administer first aid, notify parents, and EMS is called. This requires completing Sections I and III.
- Communicable Disease: A staff member is diagnosed with strep throat. All parents must be notified, and Section IV is completed.
- Risk Incident: A shelf becomes unstable and nearly falls toward a child. Even without injury, this is a reportable near-miss and must be documented.
Documents You May Need to Attach
- Doctor’s notes or parent-provided medical instructions
- Temperature logs
- First aid documentation
- Copies of email notifications to parents
- Internal incident statements from witnesses
FAQ
- Do parents always need to sign the form? Yes. Their signature confirms they received the report.
- Is this form required for minor bumps? No, only for injuries or incidents meeting HHSC reporting criteria.
- Who receives copies of the form? Parents and the operation; CCR only if the incident is reportable.
- How long must the form be kept? Operations typically retain it as part of the child’s record according to HHSC standards.
- What if a parent refuses to sign? Document the refusal and keep the form on file.
- Is electronic delivery acceptable? Yes, if accompanied by proof of how it was delivered.
Micro-FAQ
- Purpose? To document injuries, illnesses, and reportable incidents.
- Who completes it? Director or designated staff.
- When required? Medical injuries, hospitalization, communicable diseases, or risk incidents.
- Notify parents? Always for incidents; all parents for communicable diseases.
- Notify Health Department? When disease requires reporting.
- Attachments? Medical notes, emails, first aid logs.
- Submitted to CCR? Only if the event is reportable.
- Time-sensitive? Parent notification must be prompt.
- Child signature? Not required.
- Storage? Keep on file at the operation.
Related Forms
- Texas Form 2930 – Child Care Incident Reporting
- Emergency Care Authorization Form (Texas)
- Medication Authorization Form (Texas)
- Allergy and Anaphylaxis Emergency Plan
Form Details
- Name: Incident or Illness Report
- Form Number: 7239
- Region: State of Texas
- Date of Revision: October 2023