TX HHS Form 3029. Application for Program Benefits
The Application for Program Benefits (Form 3029) is a comprehensive form designed to streamline access to essential health care services for low-income individuals and families in Texas. It serves as the official application for two key programs: the Primary Health Care (PHC) Program, which provides medical and dental services to uninsured or underinsured adults and children, and the Title V Maternal & Child Health Fee-For-Service (Title V MCH FFS) Program, which focuses on prenatal, child health, and dental care for eligible pregnant women and children. This form ensures that applicants can receive fee-for-service benefits without upfront costs, based on income, residency, and other eligibility criteria. By completing it accurately, applicants can qualify for services like primary care visits, preventive screenings, family planning, and dental treatments at participating providers.
Purpose of the Form
This form is the gateway to vital health care support programs administered by the Texas Health and Human Services Commission (HHSC). Its primary purpose is to determine eligibility for free or low-cost medical, dental, and preventive services for those who might otherwise go without care due to financial barriers. The PHC Program targets adults aged 15-64 and children under 15 who are Texas residents with incomes at or below 200% of the Federal Poverty Level (FPL). The Title V MCH FFS Program extends specialized benefits to pregnant women (prenatal medical and dental care) and children up to age 21 (child health and dental services), with income limits up to 200% FPL.
By using this form, applicants can access a network of over 1,000 providers across Texas, ensuring timely care for routine check-ups, chronic condition management, immunizations, and emergency dental needs. It also screens for adjunctive eligibility, allowing automatic qualification if the household receives benefits like SNAP or WIC, bypassing detailed income verification.
Who Should Use This Form
This form is intended for:
- Low-income adults and families seeking primary health care without adequate insurance.
- Pregnant women applying for prenatal medical and dental services under Title V PMD.
- Parents or legal guardians of children under 21 needing child health and dental care under Title V CHD.
- Texas residents enrolled in other assistance programs (e.g., Medicaid, CHIP, SNAP, WIC) who may qualify adjunctively for PHC.
- Veterans and former military members, who are encouraged to note their status for potential additional benefits.
If applying for a minor, the parent or guardian must complete the form as the applicant. Unborn children of pregnant applicants must be included in household counts.
When to Use This Form
Use this form in situations where immediate or ongoing health care access is needed but financial constraints prevent it, such as:
- No health insurance or gaps in coverage, especially for dental services.
- Immediate medical or dental emergencies, where presumptive eligibility can grant temporary benefits without full documentation.
- Pregnancy, to secure prenatal care and nutritional support.
- Childhood illnesses or preventive care for uninsured kids, including immunizations and well-child visits.
- Income changes or household expansions requiring recertification every 12 months.
- Referral from a provider during a visit, or self-application at local health departments, clinics, or online via HHSC resources.
Applicants must report changes in income, address, or coverage within 30 days to maintain benefits. It's particularly crucial during open enrollment periods or when facing barriers like unemployment or family crises.
Sections of the Form
The form is divided into seven detailed sections to gather comprehensive information while ensuring privacy and compliance. Each section builds toward a complete eligibility determination.
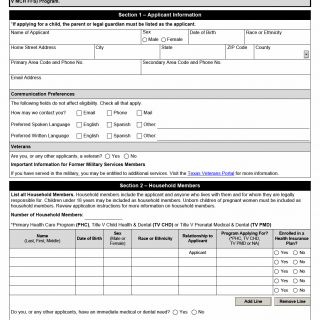
Section 1: Applicant Information
This foundational section collects personal details to identify the primary applicant. Required data includes:
- Name, sex, date of birth, race/ethnicity.
- Home address, county, primary/secondary phone numbers, email.
- Communication preferences (email, phone, mail; preferred languages for spoken/written communication).
- Veteran status, with links to Texas Veterans Portal for additional resources.
For child applications, the guardian's information is used. This section emphasizes non-discriminatory practices and accessibility.
Section 2: Household Members
Here, list all household members, defined as those living with the applicant for whom they are legally responsible. Key details per member:
- Name, date of birth, sex, race/ethnicity, relationship to applicant.
- Program applied for (PHC, Title V CHD, Title V PMD, or NA).
- Enrollment in health insurance plans.
Include unborn children for pregnant applicants. Also note immediate medical/dental needs or special circumstances (e.g., disabilities, incarceration) with explanations. Total household size is calculated here.
Section 3: Screening for PHC Adjunctive Eligibility
For PHC applicants, this screens for automatic eligibility via existing benefits:
- Check boxes for SNAP, WIC, Medicaid for Pregnant Women, or Children's Medicaid.
If verified through TMHP or TexMedConnect, skip income details. Proof of enrollment grants immediate adjunctive status.
Section 4: Household Income
Detailed financial assessment for non-adjunctive applicants. Provide:
- Per household member: Source of income, employer/payor, type (wages, self-employment, etc.), gross amount, frequency.
- Total gross monthly income, allowable deductions (e.g., child care, medical expenses), adjusted gross income.
Refer to Appendix I in the Program Policy Manual for income definitions. Documentation like pay stubs is mandatory.
Section 5: Acknowledgement
Legal affirmations include:
- Truthfulness of information and agreement to report changes.
- Privacy rights under Texas Government Code.
- Release of income/medical info to HHSC and providers.
- Attestation of no other coverage and authorization to bill listed sources.
Requires initials and signature with date.
Section 6: Contractor Eligibility Determination
Completed by eligibility staff:
- Verification of residency, income (as % of FPL), documentation for income/residency/DOB.
- Adjunctive verification and supplemental benefits (e.g., services without primary coverage).
- Screening for Medicaid/CHIP potential eligibility.
- Notes on presumptive eligibility for urgent needs.
Section 7: Contractor Eligibility Certification
Final certification by staff, including:
- Effective date, program(s), eligibility type (full or presumptive), copay amount.
- Notification of other programs and required forms (e.g., Form 3012 for eligible clients).
The form stays in client records; no submission to HHSC state office.
Requirements and Documentation
To process the application:
- Mandatory proofs: Residency (ID/utility bill), income (pay stubs/tax returns), DOB (birth certificate for Title V CHD).
- Income threshold: ≤200% FPL; no asset test.
- Residency: Texas resident only; no citizenship requirement for these programs.
- Presumptive eligibility: Granted for urgent needs without docs; full verification within 45 days.
- Dental focus: Eligible even if medical insurance exists but lacks dental.
- Recertification: Annually or upon changes.
Incomplete forms delay benefits; false info leads to disqualification and repayment.
Key Benefits and Next Steps
Approved applicants receive services at no or low copay (sliding scale based on income). Staff must inform of Medicaid/CHIP options via YourTexasBenefits.com. Track status through local contractors or HHSC portals.
Form Details
- Title: Application for Program Benefits
- Form Number: 3029
- Region/Organization: Texas Health and Human Services Commission (HHSC)
- Revision Date: November 2025
For the latest version or assistance, visit the HHSC website or contact a local eligibility contractor.