TX HHS Form 1338. Cystic Fibrosis Treatment Agents (Kalydeco/Orkambi/Symdeko) Prior Authorization Request
The TX HHS Form 1338, Cystic Fibrosis Treatment Agents Prior Authorization Request, is a crucial document for healthcare providers to request prior authorization for patients with cystic fibrosis who require treatment agents such as Kalydeco, Orkambi, or Symdeko. This form helps solve the problem of ensuring that patients receive necessary medication while also streamlining the approval process.
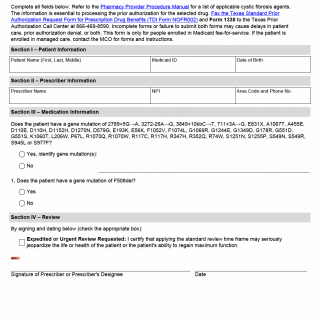
The form requires completion of three sections: Patient Information, Prescriber Information, and Medication Information. Key features include the need to identify specific gene mutations and the option for expedited or urgent review requests when patient health is at risk. The form must be faxed to the Texas Prior Authorization Call Center along with the Texas Standard Prior Authorization Request Form for Prescription Drug Benefits (TDI Form NOFROO2). Incomplete forms may cause delays in patient care, prior authorization denial, or both.
This form is only applicable for patients enrolled in Medicaid fee-for-service and not managed care. It is essential to complete all fields accurately to ensure efficient processing of the prior authorization request. Key points to note include:
- The form is used for patients with cystic fibrosis requiring treatment agents Kalydeco, Orkambi, or Symdeko.
- Completion of three sections: Patient Information, Prescriber Information, and Medication Information.
- Option for expedited or urgent review requests when patient health is at risk.
- Incomplete forms may cause delays in patient care, prior authorization denial, or both.