Praluent Appeal Letter
A Praluent appeal letter is a formal written document submitted to a health insurance company or a healthcare institution to request coverage or reimbursement for the prescription medication "Praluent." Praluent is a brand-name medication used to lower LDL cholesterol levels in individuals with specific medical conditions, such as familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease. The appeal letter is utilized when coverage for Praluent has been denied by the insurance company, and the patient or their representative believes that the medication is medically necessary for their health.
The purpose of a Praluent appeal letter is to present a compelling case to the insurance company, explaining why Praluent is a crucial and appropriate treatment option for the patient's condition. The letter aims to address the denial of coverage by providing medical evidence, physician recommendations, and other relevant information to support the claim that Praluent is necessary for the patient's well-being.
A typical Praluent appeal letter may include the following components:
-
Sender's Information: Your name, address, contact details, policy or member number (if applicable), and the date.
-
Recipient's Information: Name and address of the insurance company or relevant authority.
-
Subject Line: A concise subject indicating the purpose of the letter (e.g., "Appeal for Coverage of Praluent - Policy Number: [Your Policy Number]").
-
Salutation: A formal greeting addressing the recipient (e.g., "To Whom It May Concern,").
-
Introduction: State the purpose of the letter and explain that you are appealing the denial of coverage for Praluent.
-
Patient Information: Provide details about your medical condition, diagnosis, and the recommendation for Praluent from your healthcare provider.
-
Reasons for Appeal: Explain why Praluent is medically necessary for your condition and why it is the most appropriate treatment option.
-
Supporting Documentation: Mention that you are including relevant medical records, test results, or any other documents supporting the medical necessity of Praluent.
-
Insurance Policy Coverage: Reference the sections of your insurance policy that suggest coverage for necessary treatments and how Praluent aligns with those terms.
-
Urgency and Health Implications: Emphasize the urgency of timely treatment with Praluent to prevent health complications and highlight potential long-term health risks.
-
Request for Reconsideration: Politely request the insurance company to reconsider their decision and provide coverage for Praluent.
-
Appreciation and Additional Information: Express gratitude for their attention and offer to provide further information or clarification if needed.
-
Closing: End with a courteous closing (e.g., "Sincerely,") followed by your full name.
-
Signature: Leave space for a handwritten signature (if sending a physical letter) or a typed version of your name (if sending electronically).
-
Enclosures: List the documents you are including with the letter (e.g., "Enclosures: [List of attached medical records and test results]").
Sample of Praluent Appeal Letter
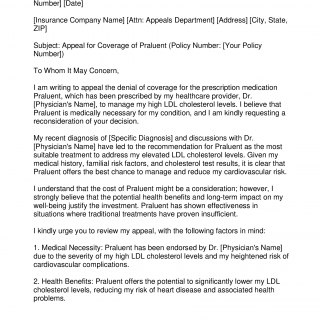
[Your Name] [Your Address] [City, State, ZIP] [Email Address] [Phone Number] [Date]
[Insurance Company Name] [Attn: Appeals Department] [Address] [City, State, ZIP]
Subject: Appeal for Coverage of Praluent (Policy Number: [Your Policy Number])
To Whom It May Concern,
I am writing to appeal the denial of coverage for the prescription medication Praluent, which has been prescribed by my healthcare provider, Dr. [Physician's Name], to manage my high LDL cholesterol levels. I believe that Praluent is medically necessary for my condition, and I am kindly requesting a reconsideration of your decision.
My recent diagnosis of [Specific Diagnosis] and discussions with Dr. [Physician's Name] have led to the recommendation for Praluent as the most suitable treatment to address my elevated LDL cholesterol levels. Given my medical history, familial risk factors, and cholesterol test results, it is clear that Praluent offers the best chance to manage and reduce my cardiovascular risk.
I understand that the cost of Praluent might be a consideration; however, I strongly believe that the potential health benefits and long-term impact on my well-being justify the investment. Praluent has shown effectiveness in situations where traditional treatments have proven insufficient.
I kindly urge you to review my appeal, with the following factors in mind:
1. Medical Necessity: Praluent has been endorsed by Dr. [Physician's Name] due to the severity of my high LDL cholesterol levels and my heightened risk of cardiovascular complications.
2. Health Benefits: Praluent offers the potential to significantly lower my LDL cholesterol levels, reducing my risk of heart disease and associated health problems.
3. Policy Compliance: My insurance policy stipulates coverage for medically necessary treatments, and Praluent aligns with this criteria as determined by Dr. [Physician's Name].
4. Urgency: Elevated LDL cholesterol levels are a recognized risk factor for heart disease, underscoring the importance of timely intervention.
Enclosed with this letter, you will find the pertinent medical records, cholesterol test results, and a comprehensive letter from Dr. [Physician's Name], outlining the rationale for Praluent as the recommended course of action. I am more than willing to provide any additional information or address any inquiries that could facilitate your review.
Thank you for your time and consideration. I remain hopeful that upon reevaluation, you will recognize the significance of Praluent in maintaining my health and well-being effectively.
Sincerely,
[Your Name]
[Your Signature]Enclosures: [List of attached medical records, cholesterol test results, and physician's letter]
A Praluent appeal letter aims to present a compelling argument for why the medication is medically necessary based on the patient's condition and healthcare provider's recommendation. It seeks to demonstrate that the benefits of Praluent outweigh any cost considerations and that coverage for the medication is essential for the patient's health and well-being.