LDSS-3634. Resident Medication Record
Form LDSS-3634, the Resident Medication Record, is a document used by staff in residential health care facilities to document medications administered to residents. It is used to ensure that all medications are administered accurately and in accordance with the specific instructions of the prescribing physician. The form is intended to be used in conjunction with other documents such as the physician’s orders, the resident’s medical record, and the facility’s medication administration policy.
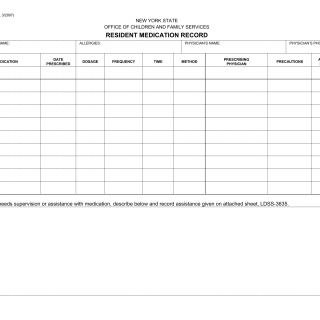
The form consists of three sections – the resident information section, the physician orders section, and the medication administration record section. The resident information section includes the name, date of birth, and room number of the resident, as well as the name and signature of the staff member administering the medication. The physician orders section contains the name, strength, and dosage of the medication, as well as the name and signature of the physician who prescribed it. The medication administration record section includes the date and time the medication was administered, the name of the staff member administering the medication, and the name and signature of the resident or guardian authorizing the medication. There is also a space to note any adverse reactions to the medication and the name and signature of the staff member documenting the reaction.
When completing the form, it is important to ensure that all information is accurate and complete. The form should be filled out at the time of administration and signed by the resident or guardian. Any adverse reactions should be documented in detail and reported to the physician. It is important that all information is recorded in accordance with the facility’s medication administration policy.
The form might be used in a residential health care facility to document the administration of medications to a resident. It provides a record of the medications that have been administered and allows for the monitoring of side effects or adverse reactions. The form also ensures that medications are administered in accordance with the instructions of the prescribing physician.
When filling out the form, it is important to ensure that all information is accurate and complete. It is also important to follow the facility’s medication administration policy and to document any adverse reactions that may occur. Related forms include the Physician’s Order for Medication, the Resident’s Medical Record, and the Facility’s Medication Administration Policy. Additional documents such as the resident’s consent forms may