Medical Appeal Letter
A medical appeal letter is a formal document that is used to appeal a decision made by a health insurance provider that denies coverage for a medical procedure, treatment or medication. The purpose of the medical appeal letter is to request the health insurance provider to reconsider the decision and provide coverage for the medical treatment that has been denied. In this article, we will provide a detailed description of the medical appeal letter, including its purpose, parts, important fields, cases in which it is compiled, parties involved, features to consider when compiling, advantages, problems that may arise, related forms and alternative forms, differences from analogues, and where and how to submit and store the form.
The purpose of the medical appeal letter is to request a health insurance provider to reconsider a decision that denies coverage for a medical procedure, treatment, or medication. The letter should provide evidence that the medical treatment is necessary for the patient's health and well-being and should be covered by the health insurance provider.
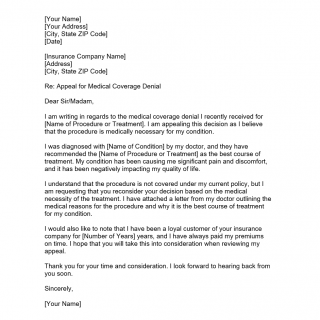
The medical appeal letter should consist of the following parts:
- Introduction: The introduction should clearly state the purpose of the letter and provide a brief overview of the medical treatment that has been denied.
- Patient Information: This section should provide the patient's name, date of birth, policy number, and other relevant information.
- Medical Information: This section should provide a detailed explanation of the medical treatment that has been denied, including the diagnosis, the recommended treatment, and the reason for the denial.
- Evidence: This section should provide evidence that the medical treatment is necessary for the patient's health and well-being and should be covered by the health insurance provider. This may include medical records, test results, and letters from healthcare providers.
- Conclusion: The conclusion should summarize the key points of the letter and request that the health insurance provider reconsider the decision.
The most important fields in the medical appeal letter are the patient's name, date of birth, policy number, and the detailed explanation of the medical treatment that has been denied. It is essential to provide evidence that the medical treatment is necessary for the patient's health and well-being and should be covered by the health insurance provider.
The medical appeal letter is compiled when a health insurance provider denies coverage for a medical procedure, treatment, or medication. The parties involved are the patient, healthcare provider, and the health insurance provider.
When compiling the medical appeal letter, it is essential to consider the following features:
- The letter should be concise, professional, and to the point.
- Provide clear evidence that the medical treatment is necessary for the patient's health and well-being.
- Use a polite and respectful tone.
- Include all relevant information, including medical records, test results, and letters from healthcare providers.
The medical appeal letter has several advantages, including:
- It provides an opportunity to request that the health insurance provider reconsider a decision that denies coverage for a medical procedure, treatment, or medication.
- It provides evidence that the medical treatment is necessary for the patient's health and well-being.
- It can potentially save the patient from having to pay for the medical treatment out of pocket.
Some problems that may arise when filling out the medical appeal letter include:
- Lack of clear evidence that the medical treatment is necessary for the patient's health and well-being.
- The letter is not concise, professional, or to the point.
- The tone of the letter is not polite or respectful.
- The letter is missing relevant information, such as medical records, test results, and letters from healthcare providers.
Related Forms and Alternative Forms, as well as Differences from Analogues
Related forms to the medical appeal letter include the Explanation of Benefits (EOB) form and the Prior Authorization form. The EOB form is used to explain the benefits and coverage provided by the health insurance provider for a specific medical procedure, treatment, or medication. The Prior Authorization form is used to request approval from the health insurance provider for a specific medical procedure, treatment, or medication.
Differences from analogues are that the medical appeal letter is used to appeal a decision that denies coverage for a medical procedure, treatment, or medication, while the EOB form and the Prior Authorization form are used to explain benefits and request approval for medical procedures, treatments, or medications.
The medical appeal letter should be submitted to the health insurance provider either through mail or email. It is recommended to keep a copy of the letter for personal records. The health insurance provider will keep a copy of the letter in the patient's file.
The medical appeal letter is a formal document used to appeal a decision made by a health insurance provider that denies coverage for a medical procedure, treatment, or medication. The letter should provide clear evidence that the medical treatment is necessary for the patient's health and well-being and should be covered by the health insurance provider. It is essential to be professional, concise, and to the point when compiling the letter. The medical appeal letter can potentially save the patient from having to pay for the medical treatment out of pocket.