CMS 10123. FFS & MA NOMNC/DENC
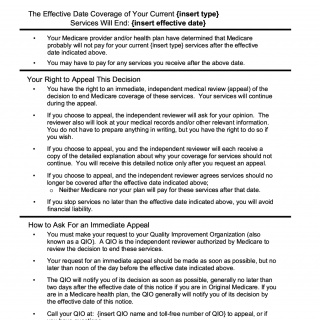
The FFS & MA NOMNC/DENC form is used to notify Medicare beneficiaries of their right to appeal a decision regarding their Medicare coverage. The form consists of several parts, including a notice of Medicare non-coverage (NOMNC) or denial (DENC), an explanation of the reasons for the decision, and instructions for filing an appeal.
- FFS - Fee-for-Service: This refers to the traditional Medicare program, where healthcare providers are paid a fee for each service they provide to a Medicare beneficiary. In the FFS program, beneficiaries can choose to receive care from any Medicare-approved provider who accepts Medicare payment terms and conditions.
- MA - Medicare Advantage: This refers to the Medicare program that allows beneficiaries to receive their Medicare benefits through private health insurance plans, such as Health Maintenance Organizations (HMOs) or Preferred Provider Organizations (PPOs). These plans are offered by private insurance companies that are approved by Medicare and provide all the same benefits as the traditional Medicare program, plus additional benefits like prescription drug coverage, vision, and dental care.
- NOMNC - Notice of Medicare Non-Coverage: This refers to a notice that is given to Medicare beneficiaries who are receiving services that are not covered by Medicare. The notice explains why the services are not covered and informs the beneficiary of their right to appeal the decision.
- DENC - Detailed Explanation of Non-Coverage: This refers to a more detailed notice that is given to Medicare beneficiaries who have already received a NOMNC and have chosen to appeal the decision. The DENC provides additional information about the decision and the appeals process, including the beneficiary's right to a hearing.
Important fields on the form include the beneficiary's name, Medicare number, the date of the notice, and the reason for the decision. The parties involved in the form include the Medicare beneficiary, their healthcare provider, and the Centers for Medicare & Medicaid Services (CMS).
When compiling the form, the beneficiary will need to provide their personal information, such as their name and Medicare number, as well as information about the healthcare services they received. No additional documents are required to be attached to the form.
An example of a practice use case for the FFS & MA NOMNC/DENC form is when a Medicare beneficiary receives a notice of non-coverage or denial for a particular healthcare service and wishes to appeal the decision.
Strengths of the form include providing beneficiaries with a clear explanation of the reasons for the decision and instructions for filing an appeal. Weaknesses include the potential for confusion or misunderstanding regarding the appeals process.
An alternative form to the FFS & MA NOMNC/DENC is the CMS-1696 form, which is used for filing a Medicare appeal for services that have already been received. The main difference between the two forms is that the FFS & MA NOMNC/DENC is used for notifying beneficiaries of a decision, while the CMS-1696 is used for filing an appeal after the fact.
Submitting the form typically involves mailing it to the address provided on the form. The form is stored in the beneficiary's CMS file as well as in the healthcare provider's records.
Overall, the FFS & MA NOMNC/DENC form plays a crucial role in ensuring that Medicare beneficiaries are informed of their right to appeal a decision regarding their healthcare coverage, and provides clear instructions for doing so.