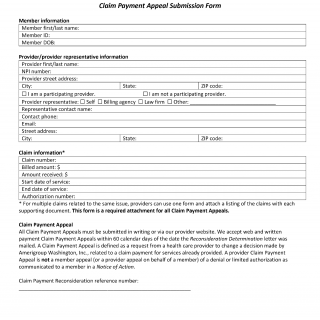
Amerigroup Claim Payment Appeal Submission Form
The Claim Payment Appeal Submission Form is a crucial document that enables healthcare providers to formally challenge decisions made by Amerigroup Washington, Inc. regarding claim payments for services rendered. This form serves as a means to rectify payment discrepancies and ensure accurate compensation for provided healthcare services. By providing comprehensive member and provider information, as well as detailing the reason for the appeal, this form initiates the process of addressing claim payment disputes in a structured and organized manner.
Important Parts:
-
Member Information: This section captures essential details about the member, including their first and last name, member ID, and date of birth.
-
Provider/Provider Representative Information: This part requires information about the healthcare provider or their representative. It includes options for identifying whether the provider is participating, the representative's contact details, and their relationship to the provider (e.g., self, billing agency, law firm).
-
Claim Information: This section gathers specifics related to the claim being appealed, such as claim number, billed and received amounts, start and end dates of service, and authorization number. For multiple related claims, providers can use this form with a list of claims and supporting documents.
-
Claim Payment Appeal: This segment outlines the scope and nature of a Claim Payment Appeal. It clarifies that a Claim Payment Appeal involves changing a payment decision for services already provided, distinct from member appeals or denials related to limited authorization.
-
Reason for Claim Payment Appeal: This section provides checkboxes for various reasons for the appeal, including issues like untimely filing, lack of authorization, denial due to other health insurance, experimental/investigational procedure denial, claim code editing denial, and more.
Parties Involved:
- Member: The individual who received the healthcare services covered by the claim and whose claim payment is under dispute.
- Provider/Provider Representative: The healthcare provider or their representative (billing agency, law firm, etc.) appealing the claim payment decision.
- Amerigroup Washington, Inc.: The insurance company that made the original claim payment decision and is responsible for reviewing the appeal.
Case Example:
Suppose Dr. Smith, a healthcare provider, rendered medical services to a member covered by Amerigroup Washington, Inc. However, there was a discrepancy in the claim payment amount. Dr. Smith believes that the payment received does not accurately reflect the services provided. Dr. Smith decides to use the Claim Payment Appeal Submission Form to formally challenge the payment decision, ensuring that the services rendered are adequately compensated.
By completing the form with accurate member and provider information, specifying the reason for the appeal (perhaps "Disagree that you were paid according to contract"), and submitting supporting documentation, Dr. Smith initiates the process of addressing the payment discrepancy. Amerigroup Washington, Inc. will then review the appeal and take appropriate action to ensure that the correct payment is made to Dr. Smith for the services provided.
The Claim Payment Appeal Submission Form acts as a bridge between healthcare providers and insurance companies, facilitating the resolution of claim payment disputes. Through a clear and organized format, this form empowers providers to present their case, outline the reasons for their appeal, and ensure accurate and fair compensation for the healthcare services they deliver.