CMS-588 Electronic Funds Transfer (EFT) Authorization Agreement
The CMS-588 form is the Electronic Funds Transfer (EFT) Authorization Agreement form, used by healthcare providers to authorize electronic payments from Medicare to their designated bank account.
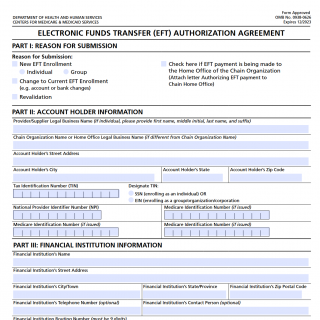
The form consists of several parts, including general information about the healthcare provider or supplier, bank account information, and signature and certification statements. The most important fields in the form include the provider's name, National Provider Identifier (NPI) number, and bank account information.
This form is compiled by healthcare providers who wish to receive electronic payments for services provided to Medicare beneficiaries. The parties involved in this document are the healthcare provider or supplier and the Centers for Medicare & Medicaid Services (CMS).
When compiling this form, it is important to ensure that all information provided is accurate and up-to-date, particularly bank account information. The provider should also carefully review and agree to all signature and certification statements included in the form.
The advantages of this form include the ability for healthcare providers to receive electronic payments from Medicare, which can save time and reduce administrative costs associated with paper checks. However, problems can arise when filling out the form if the bank account information provided is inaccurate or incomplete, which can result in delays or errors in payment processing.
Related forms include the CMS-855I Medicare Enrollment Application for individual providers, the CMS-855B Medicare Enrollment Application for group practices, and the CMS-855R Medicare Enrollment Application for reassignment of benefits. Alternative forms include paper forms for submitting payment information, such as the CMS-855P Medicare Enrollment Application for institutional providers. The main difference between these forms is the type of information they are intended to collect.
The CMS-588 form can be submitted electronically through the Medicare Administrative Contractor (MAC) for the provider's state or by mail to the Medicare contractor handling the provider's claims. The form should be stored in a secure location to ensure confidentiality of the information provided.