Aetna Practitioner and Provider Complaint and Appeal Request Form (GR-69140)
The Practitioner and Provider Complaint and Appeal Request form is an essential tool provided by Aetna to facilitate the process of addressing concerns, disputes, and appeals related to medical or dental services provided within their network. This form is designed to assist both practitioners/providers and members in communicating their grievances and seeking resolution for denied claims or unfavorable decisions.
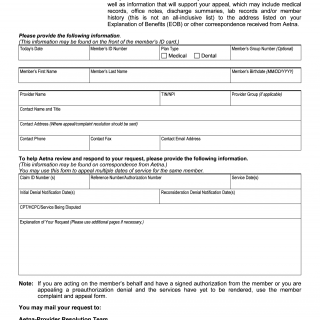
Form Details: Completion of this form is mandatory for individuals seeking a review of their appeal or complaint. It is necessary to accompany this form with pertinent supporting documents such as medical records, office notes, discharge summaries, lab records, and other relevant information that substantiates the appeal request. The form includes spaces for the following information:
- Today's Date: The date on which the form is being completed.
- Member's ID Number: The unique identification number of the member, often found on their ID card.
- Plan Type: Whether the claim pertains to medical or dental services.
- Member's Group Number (Optional): The group number associated with the member, if applicable.
- Member's First Name: The first name of the member.
- Member's Last Name: The last name of the member.
- Member's Birthdate: The birthdate of the member in MM/DD/YYYY format.
- Provider Name: The name of the healthcare provider involved.
- TIN/NPI: Tax Identification Number (TIN) or National Provider Identifier (NPI) of the provider.
- Provider Group (if applicable): The group or practice to which the provider belongs.
- Contact Information: Name, title, address, phone number, fax, and email address of the person who will handle the appeal/complaint resolution.
- Claim Details: Information relevant to the claim being disputed, including Claim ID Number(s), Reference Number/Authorization Number, Service Date(s), Initial Denial Notification Date(s), Reconsideration Denial Notification Date(s), and CPT/HCPC/Service Being Disputed.
- Explanation of Your Request: A space for the individual to explain the reasons for their appeal or complaint. Additional pages can be used if necessary.
- Note: Guidance for cases where the individual is acting on behalf of the member or is appealing a preauthorization denial before services have been rendered.
Submission Options: The completed form and supporting documents can be submitted by mail to the Aetna-Provider Resolution Team at the provided address: Aetna-Provider Resolution Team PO Box 14020 Lexington, KY 40512
Alternatively, the documents can be sent through the national fax number: 859-455-8650.
The Practitioner and Provider Complaint and Appeal Request form serves as a structured and organized way for both practitioners/providers and members to address disputes and appeals, ensuring that all relevant information is provided for a comprehensive review by Aetna's resolution team.