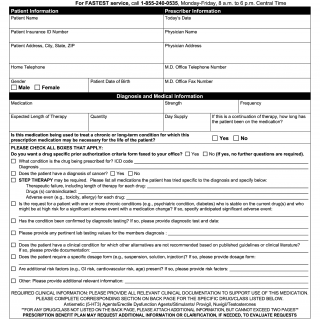
Aetna Medical Exception / Prior Authorization / Precertification Request Form for Prescription
The Aetna Medical Exception/Prior Authorization/Precertification Request Form for Prescription is a pivotal document designed to facilitate the authorization process for specific prescription medications under the Aetna insurance plan. This form streamlines the procedure of requesting authorization for medications that require further evaluation due to factors such as medical necessity, treatment alternatives, and insurance coverage criteria.
Submitting the Form:
- The completed form can be submitted via fax to the designated number: 1-877-269-9916.
- Alternatively, for expedited and convenient submission, the form can be completed and submitted online at www.availity.com.
Accessing Information:
- The form provides a reference to access essential information regarding medications and pharmacy clinical policy bulletins by visiting www.aetna.com/formulary.
Rapid Service Assistance:
- For the swiftest service, healthcare professionals can call 1-855-240-0535 between Monday and Friday, from 8 a.m. to 6 p.m. Central Time.
Patient Information:
- Commencing with the patient's name, insurance ID number, address, telephone number, gender, and date of birth, this section captures key patient details.
Prescriber Information:
- The prescriber's name, office telephone number, and fax number are documented for communication purposes.
Diagnosis and Medical Information:
- This section records the medication details, including its name, strength, frequency of use, expected length of therapy, quantity, and day supply.
- For ongoing therapy, the form inquires about the duration the patient has been on the medication.
- An essential query involves whether the medication is being utilized to treat a chronic or long-term condition that necessitates continuous use.
- A set of checkboxes allows identification of the nature of the diagnosis and the potential requirement for step therapy.
Clinical Documentation and Attachments:
- The form emphasizes the need for relevant clinical documentation to substantiate the requested medication's use.
- A section on the back page allows for the provision of specific information for certain drug/classes listed, such as Antiemetic (5-HT3) Agents, Erectile Dysfunction Agents, Stimulants, Provigil, Nuvigil, and Testosterones.
- For drugs/classes not listed, there is the option to attach additional information, with a restriction of a maximum of two pages.
Urgent Requests and Attestation:
- A section is dedicated to indicating an urgent request, signifying cases where a standard review timeframe might seriously endanger the patient's health.
- The prescriber attests to the medical necessity of the requested medication, the accuracy of the information provided, and the availability of supporting documentation.
- The form concludes with the prescriber's signature and the date, finalizing the attestation.
Confidentiality Notice:
- The form ends with a confidentiality notice, underlining the privileged and confidential nature of the transmitted health information.
In summary, the Aetna Medical Exception/Prior Authorization/Precertification Request Form for Prescription is an instrumental tool in expediting the process of medication authorization. It ensures that patients receive the appropriate medications within the parameters of their insurance coverage, while also maintaining communication and transparency between healthcare professionals and insurance providers. This form underscores the significance of coordination in delivering effective medical care.