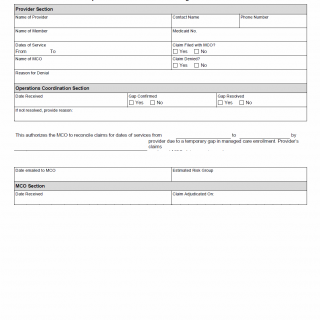
TX HHS Form H2064. Gap in Enrollment for Medicaid Managed Care Members
The TX HHS Form H2064, "Gap in Enrollment for Medicaid Managed Care Members," is a crucial document that helps resolve issues related to temporary gaps in managed care enrollment. This form is typically used by healthcare providers who need to reconcile claims for dates of service during a brief period when a patient's managed care enrollment was interrupted.
This form requires the provider to specify the dates of service, claim filing information, and the name of the Medicaid Managed Care Organization (MCO) involved. The form also includes sections for operations coordination, including the date received, gap confirmed, and gap resolved. By completing this form, providers can ensure that claims are accurately processed and patients receive the necessary medical attention without delays.
Key features of this form include:
- The need to specify dates of service and claim filing information
- The requirement for provider's name and MCO information
- The importance of operations coordination, including date received, gap confirmed, and gap resolved