Out-of-network Appeal Letter
An out-of-network appeal letter is a formal written request made by a patient or their healthcare provider to an insurance company. The purpose of the letter is to challenge a denial or reduction of coverage for medical services received from a healthcare provider who is not part of the insurance company's established network.
When a patient receives medical care from an out-of-network provider, the insurance company may deny coverage or provide only partial reimbursement, leaving the patient with higher out-of-pocket costs. An appeal letter is a way to contest this decision by providing additional information and documentation to support the case for coverage.
Here are the key components typically included in an out-of-network appeal letter:
-
Patient Information: Include the patient's name, policy number, and contact information.
-
Description of Services: Clearly state the medical services that were received from the out-of-network provider, including dates, descriptions of procedures, and any relevant medical codes.
-
Reason for Out-of-Network Services: Explain why the services were obtained from an out-of-network provider. This might involve providing information about the medical necessity of the services, the unavailability of appropriate in-network providers, or other extenuating circumstances.
-
Documentation: Attach copies of relevant medical records, test results, doctor's notes, and any other supporting documentation that demonstrates the medical necessity of using the out-of-network provider.
-
Provider's Letter: If applicable, include a letter from the treating physician or specialist explaining why the out-of-network care was necessary and how it was in the patient's best medical interest.
-
Policy Information: Reference the specific sections of the insurance policy that pertain to out-of-network coverage, including any exceptions or conditions where coverage might be granted.
-
Cost Considerations: If the patient faced financial hardship or inconvenience in accessing in-network care, explain these factors and how they contributed to the decision to seek out-of-network services.
-
Request for Reconsideration: Clearly state the desired outcome, whether it's a request for partial or full reimbursement of the out-of-network costs, or a request for the insurance company to reconsider the coverage decision.
-
Contact Information: Provide contact information for the patient, their healthcare provider, and any other relevant parties involved in the appeal process.
-
Signature: The letter should be signed by the patient or their authorized representative.
It's important to review the insurance company's guidelines for submitting appeals, as they may have specific procedures and deadlines that need to be followed. Crafting a well-structured and informative appeal letter with supporting documentation can significantly increase the chances of a successful outcome in challenging the denial or reduction of coverage for out-of-network services.
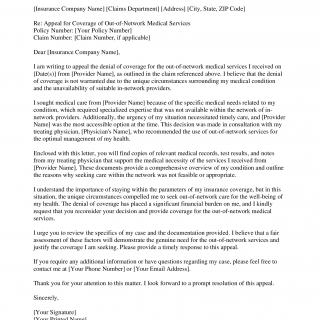
[Your Name] [Your Address] [City, State, ZIP Code] [Date]
[Insurance Company Name] [Claims Department] [Address] [City, State, ZIP Code]
Re: Appeal for Coverage of Out-of-Network Medical Services
Policy Number: [Your Policy Number]
Claim Number: [Claim Number, if applicable]Dear [Insurance Company Name],
I am writing to appeal the denial of coverage for the out-of-network medical services I received on [Date(s)] from [Provider Name], as outlined in the claim referenced above. I believe that the denial of coverage is not warranted due to the unique circumstances surrounding my medical condition and the unavailability of suitable in-network providers.
I sought medical care from [Provider Name] because of the specific medical needs related to my condition, which required specialized expertise that was not available within the network of in-network providers. Additionally, the urgency of my situation necessitated timely care, and [Provider Name] was the most accessible option at the time. This decision was made in consultation with my treating physician, [Physician's Name], who recommended the use of out-of-network services for the optimal management of my health.
Enclosed with this letter, you will find copies of relevant medical records, test results, and notes from my treating physician that support the medical necessity of the services I received from [Provider Name]. These documents provide a comprehensive overview of my condition and outline the reasons why seeking care within the network was not feasible or appropriate.
I understand the importance of staying within the parameters of my insurance coverage, but in this situation, the unique circumstances compelled me to seek out-of-network care for the well-being of my health. The denial of coverage has placed a significant financial burden on me, and I kindly request that you reconsider your decision and provide coverage for the out-of-network medical services.
I urge you to review the specifics of my case and the documentation provided. I believe that a fair assessment of these factors will demonstrate the genuine need for the out-of-network services and justify the coverage I am seeking. Please provide a timely response to this appeal.
If you require any additional information or have questions regarding my case, please feel free to contact me at [Your Phone Number] or [Your Email Address].
Thank you for your attention to this matter. I look forward to a prompt resolution of this appeal.
Sincerely,
[Your Signature]
[Your Printed Name]
Submitting a well-constructed appeal letter with proper documentation can increase the chances of the insurance company reconsidering their coverage decision and providing reimbursement for the out-of-network services. It's important to review the specific guidelines provided by the insurance company for submitting appeals and to follow their procedures closely.