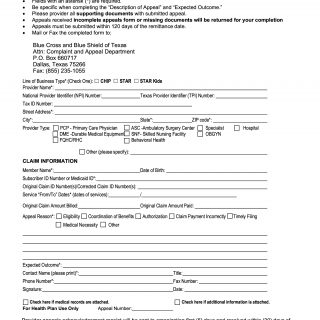
BCBS Provider Appeal Request Form
The Provider Appeal Request Form is a formal document designed for healthcare providers to initiate the process of appealing a previously adjudicated or paid claim with Blue Cross and Blue Shield of Texas. This form serves as a crucial communication tool between healthcare providers and the insurance company, enabling providers to seek a reevaluation of claim-related decisions. The form outlines essential instructions and fields to be completed, ensuring a comprehensive and organized submission of the appeal request.
Key Instructions and Information:
-
Submission Format: The form emphasizes the need for individual submission for each member requiring an appeal of an adjudicated/paid claim.
-
Required Fields: Fields marked with an asterisk (*) are mandatory to complete. This ensures that essential information is provided for a thorough understanding of the appeal.
-
Clarity and Specificity: Providers are encouraged to provide clear and specific information in the "Description of Appeal" and "Expected Outcome" sections. This helps the insurance company understand the context and purpose of the appeal.
-
Supporting Documents: Providers are required to submit all relevant supporting documents along with the appeal form. These documents are essential for the accurate evaluation of the appeal.
-
Completeness of Submission: Incomplete appeals forms or missing documents will be returned to the provider for completion, delaying the appeal process.
-
Submission Deadline: Appeals must be submitted within 120 days of the remittance date, ensuring a timely resolution of disputes.
-
Submission Options: Providers can submit the completed form and supporting documents either by mail or fax to the designated addresses provided on the form.
Claim Information Section:
-
Providers need to provide member-specific details, including the member's name, date of birth, and subscriber or Medicaid ID.
-
Information related to the original claim, such as claim ID numbers, service dates, billed amount, and paid amount, is to be specified.
-
The "Appeal Reason" section allows providers to select the specific reason for the appeal from options such as eligibility, coordination of benefits, claim payment incorrectly, timely filing, medical necessity, and others.
-
The "Expected Outcome" section should clearly outline the anticipated resolution or outcome the provider is seeking through the appeal.
Contact Information:
-
Providers need to provide their contact information, including name, title, phone number, and fax number.
-
A signature and date field is provided for authentication purposes.
-
Checkbox options are available to indicate if medical records or additional information are attached to the appeal.
For Health Plan Use Only:
- The form includes a space for an appeal number, which is assigned by the health plan upon receipt.
Acknowledgment and Resolution:
-
The form states that an acknowledgment receipt will be sent to the organization within five days of receipt. Additionally, it specifies that provider appeals will be resolved within 30 days of receipt.
-
Providers are reminded that this form is not intended for claims reconsideration and are directed to use the claims reconsideration process available on the Blue Cross and Blue Shield of Texas website.
Overall, the Provider Appeal Request Form provides a structured and organized approach for healthcare providers to formally appeal claim-related decisions, promoting clear communication and facilitating a fair review process.