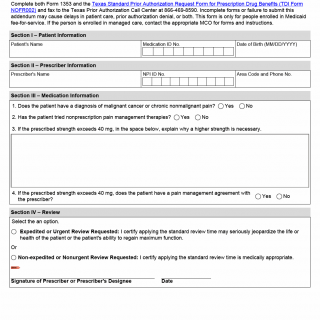
TX HHS Form 1353. Texas Medicaid OxyContin Prior Authorization Request
The Texas Medicaid OxyContin Prior Authorization Request Form 1353 helps healthcare providers obtain approval for patients' prescriptions of OxyContin. This form is specifically designed for patients enrolled in Medicaid fee-for-service and is used to request prior authorization for the medication.
This form requires prescribers to provide specific information about the patient's condition, including a diagnosis of malignant cancer or chronic nonmalignant pain, attempts at nonprescription pain management therapies, and the necessity of a higher strength dosage. Additionally, the form asks if the patient has a pain management agreement with their prescriber. The prescriber must also select an option for review, either expedited or non-expedited, depending on the urgency of the situation.
Key features of this form include the required information and conditions listed above. It is essential to complete both Form 1353 and the Texas Standard Prior Authorization Request Form for Prescription Drug Benefits (TDI Form) and fax them to the Texas Prior Authorization Call Center at 866-469-8590. Failure to submit a complete form may result in delays, denial of prior authorization, or both.
- This form is only for patients enrolled in Medicaid fee-for-service.
- Prescribers must provide specific information about the patient's condition and treatment plan.
- The form requires selection of an option for review: expedited or non-expedited.