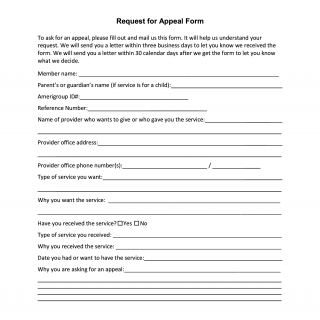
Amerigroup Request for Appeal Form
The Request for Appeal Form serves as a vital tool for individuals seeking to initiate an appeal process for denied or disputed services. Through this form, members communicate their desire for an appeal, provide essential information about the service in question, and explain the reasons for the appeal. This comprehensive form ensures that the necessary details are provided to facilitate a prompt and fair resolution.
Important Parts:
-
Member Information: This section collects the member's name and, if applicable, the parent's or guardian's name if the service is for a child. The Amerigroup ID# and a reference number are also included to ensure accurate identification.
-
Provider Information: This part requires details about the healthcare provider who administered or intends to administer the service. This information helps in understanding the context of the appeal.
-
Type of Service: Members specify the type of service they want or received, accompanied by a description of why they are seeking this service.
-
Service Details: Members indicate whether they have already received the service and, if so, describe the type of service received and the reason for it. Dates related to the service are provided to establish a timeline.
-
Reason for Appeal: This segment allows members to articulate the reasons for requesting an appeal. It is a crucial section for explaining why the member believes the service should be approved.
-
Signature and Contact: The member or an authorized representative signs the form. Contact information for the provider's office and the member services hotline is provided for additional assistance.
Parties Involved:
- Member: The individual seeking the appeal, either for themselves or on behalf of a child.
- Provider: The healthcare provider who delivered or intends to deliver the service that is being appealed.
- Amerigroup Iowa, Inc.: The healthcare insurance company that will review the appeal and make a decision based on the provided information.
Case Example:
Consider a scenario in which a member named Sarah requires a specific medical procedure that her healthcare provider, Dr. Johnson, recommends. However, the procedure was denied by Amerigroup Iowa, Inc. due to coverage limitations. Sarah firmly believes that the procedure is necessary for her health and well-being.
In response, Sarah completes the Request for Appeal Form. She includes her name, Amerigroup ID#, and the reference number provided by Amerigroup. She describes the procedure, its importance, and the reasons she is seeking the appeal. Dr. Johnson provides information about his office, and Sarah signs the form. The form is then sent to Member Grievances and Appeals at Amerigroup Iowa, Inc.
Amerigroup reviews the form and investigates Sarah's case. After a thorough evaluation, Amerigroup communicates its decision within 30 calendar days. If the appeal is successful, Sarah can proceed with the recommended medical procedure.
The Request for Appeal Form empowers members to advocate for their healthcare needs by initiating an appeal process. By providing comprehensive details about the service, reasons for appeal, and necessary signatures, members ensure that their case is thoroughly reviewed by the insurance company. This form plays a pivotal role in facilitating communication between members, providers, and the insurance company in pursuit of fair and appropriate healthcare services.